Anesthesia and the Autistic Child

All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
If your child is about to have surgery or needs a particular diagnostic procedure, such as a GI scope, their medical team will need to place them under sedation. Additionally, some children require sedation to have their teeth cleaned or a cavity filled because anxiety/sensory issues prevent them from obtaining routine dental care. Because anesthesia can exacerbate underlying health problems common to autism, deciding whether or not to have your child sedated for dental and diagnostic procedures can be stressful. But, it’s important to know that with the proper precautions, kids with autism can be sedated safely.
In this article, we will discuss:
- The difference between sedation, general anesthesia, and local anesthesia
- Underlying health conditions, common to autism, that anesthesia exacerbates
- Things to discuss with your child’s medical team before any procedure
- Common anesthetics to be aware of
Sedation, General Anesthesia, & Local Anesthesia
Before we talk about medications used for anesthesia, let’s briefly discuss the difference between sedation, general anesthesia, and local anesthesia.
Sedation
Sedation, also known as Twilight Sleep or Monitored Anesthesia Care (MAC), is when doctors use small doses of anesthesia to block pain, reduce anxiety, and help patients feel comfortable during and after procedures.
- Levels of sedation can range from minimal (the patient feels tired but able to talk) to deep (the patient probably won’t remember the procedure).
- Sedation is typically used with shorter surgeries or outpatient procedures, such as a colonoscopy.
General Anesthesia
General anesthesia is a combination of medications that put your child in a sleep-like state before a medical procedure.
- While your child is under general anesthesia, they are entirely unconscious.
- As a safety precaution, the anesthesia team will place a breathing tube while your child is under the influence of general anesthesia.
Local Anesthesia
Local anesthetics are given as an injection directly to an area that needs to be numb, such as a tooth that needs a cavity filled or a finger that needs stitches.
Common Co-Occurring Health Conditions Anesthesia Exacerbates
Many children with autism have underlying medical issues; among the most common are mitochondrial dysfunction and methylation abnormalities. Unfortunately, children with either of these conditions are more prone to regression post-anesthesia. Below we will discuss why this happens.
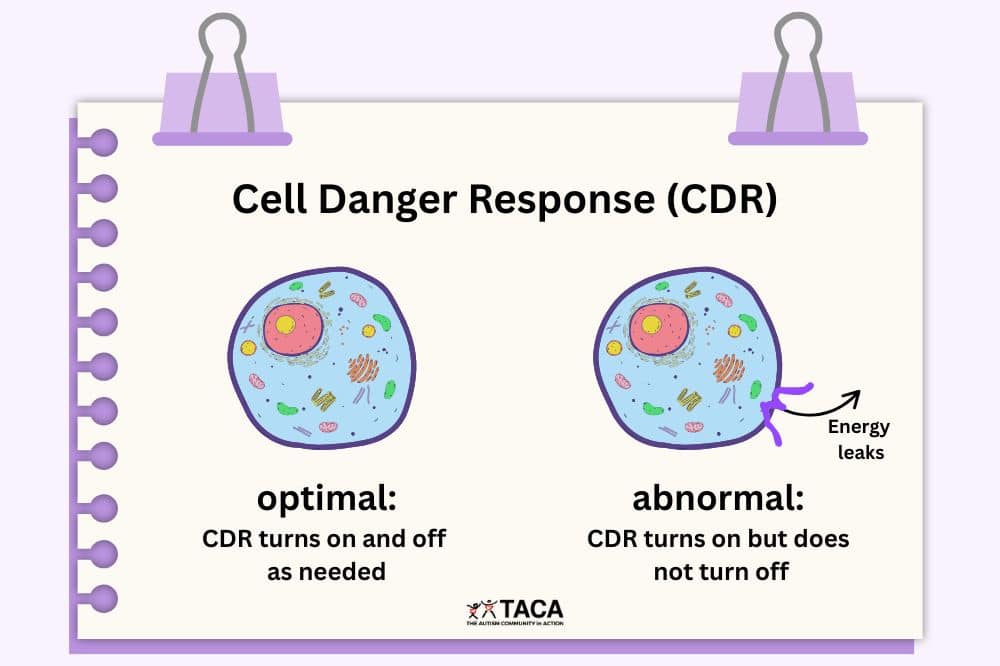
Mitochondrial Dysfunction
Because many anesthetics function in the mitochondria of the cell, they can compound issues related to Mitochondrial Dysfunction. For example, some anesthetics can affect the mitochondria’s structure or lower the cell’s ability to produce energy. Consequently, a potential adverse reaction to anesthesia is regression if proper precautions are not taken.
Methylation Abnormalities
Another common co-occurring condition in autism that anesthesia exacerbates involves methylation abnormalities. Methylation is a primary way the body rids itself of toxins. Therefore, if your child has methylation abnormalities, their ability to detoxify anesthetics after their procedure will be further impaired.
Considerations for Children with Mitochondrial Dysfunction and Methylation Abnormalities
In order to mitigate adverse effects from anesthesia medications, individuals with mitochondrial dysfunction and methylation abnormalities should consider avoiding certain medications.
When discussing anesthesia options with your child’s doctor, please consider the following:
- Local Anesthesia:
- Lidocaine is the preferred local anesthetic because it’s less harmful to the mitochondria (it inhibits carnitine to a lesser degree than bupivacaine).
- Sedation:
- This study indicates that small doses of Ketamine won’t cause mitochondrial damage (more information about Ketamine below).
- If your child needs to be sedated for more than 20 minutes, consider avoiding Propofol (more details about Propofol below).
- Hydration During Surgery:
- Lactated Ringer’s solution (LR) is an IV solution doctors use to treat dehydration or administer IV medications during surgery.
- Because it has many of the same electrolytes as blood, some doctors prefer it to regular saline.
- However, individuals with mitochondrial dysfunction should avoid Lactated Ringer’s solution because it can elevate blood lactate levels, further impairing mitochondrial function.
- Instead, doctors should administer regular saline IV fluids to patients with mitochondrial dysfunction.
- Lactated Ringer’s solution (LR) is an IV solution doctors use to treat dehydration or administer IV medications during surgery.
Detoxification Support for Children with Mitochondrial Dysfunction and Methylation Abnormalities
Additionally, children with mitochondrial dysfunction and metabolic abnormalities may need supplemental support to detoxify anesthetics in a timely manner.
Accordingly, your child’s functional medicine doctor may suggest adding one or more of the following supports before/after any surgical procedure:
- Overall Detoxification Support:
- Hydration with filtered water
- Plenty of rest
- Epsom salt baths
- Epsom salts contain sulfate, which aids in the detoxification process.
- Antioxidants
- CoQ10
- L-Carnitine
- Vitamin E
- Vitamin C
- Mitochondrial Support:
- Thiamine (B1)
- Pantothenic Acid (B5)
- Pyridoxine (B6)
- Biotin (B7)
- Alpha Lipoic Acid
- This research paper titled Primary Mitochondrial Disease and Secondary Mitochondrial Dysfunction: Importance of Distinction for Diagnosis and Treatment gives a breakdown of the mitochondrial cocktail.
- Methylation Support:
- Methyl B12
- Methylfolate (5MTHF, folinic acid)
- N-acetyl-L-cysteine
- Zinc
- BH4
What to Discuss with Your Child’s Medical Team Before any Procedure
Establishing a direct and open communication line between you, the prescribing physician, and the anesthesia team is an essential part of preparing for a safe and comfortable procedure. The following are a few examples of things to discuss with your child’s team before the procedure:
- Past Responses:
- If your child has reacted poorly to anesthesia in the past, please convey that to the anesthesia team, so they know your child’s complete history and can make better choices for your child this time.
- Twilight vs. General Anesthesia:
- Ask your doctor if your child simply needs sedation or if they require general anesthesia, which requires a breathing tube.
- Fasting:
- Most procedures with anesthesia will require fasting, which can be a problem for children with low blood sugar, metabolic issues, or mitochondrial dysfunction. If your child has one of these medical issues, prepare to discuss them with the prescribing doctor. If necessary, the anesthesia team can administer IV dextrose to mitigate any side effects of the fasting.
- Location:
- Always sedate in a hospital setting. It is safer, and they have personnel with access to medications and equipment in case of an emergency.
Common Anesthetics
In order to help you make an educated decision in conjunction with your child’s medical team, let’s overview the characteristics of some anesthesia medications doctors commonly use.
For your convenience, medications are listed in alphabetical order.
Desflurane
This is a highly fluorinated methyl ethyl ether used for the maintenance phase of general anesthesia.
- Precaution:
- Studies show that Desflurane causes significant oxidative stress.
- Already a known problem in autism, oxidative stress can cause fatigue, memory loss, headaches, joint pain, and numerous chronic diseases.
- Studies show that Desflurane causes significant oxidative stress.
Fentanyl
This sedative is a short-acting opioid.
- Fentanyl tends to be well tolerated.
Ketamine
Ketamine is a sedative that puts patients in a trance-like state, causing them to forget what happened.
- This study indicates that small doses of Ketamine don’t cause mitochondrial damage.
- Precautions:
- Due to metabolic differences, sometimes Ketamine has no sedative effect on a small percentage of kids with autism.
- Additionally, some kids with autism take longer to wake in the recovery room after being sedated with Ketamine.
Nitrous Oxide (N2O)
This sedative agent is also known as “laughing gas.”
- Precautions:
- Individuals with vitamin B12 deficiencies, an underlying medical condition common to autism, may want to avoid Nitrous Oxide for the following reasons:
- Also, this study indicates that Nitrous Oxide has the potential to exacerbate autism symptoms.
Precedex (Dexmedetomidine)
This sedative agent stops the release of norepinephrine which blocks pain signals. It also decreases blood pressure and heart rate.
- Precedex tends to be well tolerated by most kids with autism if general anesthesia is needed.
- It does not cause respiratory depression, so anesthesiologists favor it.
- Precaution:
- Some kids with autism take longer to wake in the recovery room when using Precedex.
Propofol
This short-acting anesthetic quickly transitions patients from a conscious to a sedated state by slowing the activity of the brain and nervous system.
- It can be acceptable if sedated for less than 20 minutes.
- Precautions:
- If Propofol is used for more than 20 minutes, it is toxic to the mitochondria.
- For instance, Propofol is unique because it affects mitochondrial metabolism by at least four separate mechanisms.
- Also, children with food allergies/sensitivities to soy or egg need to avoid Propofol because it is mixed in a liquid that contains soybean oil and egg lecithin.
- Additionally, patients with a history of atopy (a tendency to produce an exaggerated immunoglobulin E (IgE) immune response) are more likely to have an allergic reaction to Propofol.
- If Propofol is used for more than 20 minutes, it is toxic to the mitochondria.
Sevoflurane Without Nitrous Oxide
Sevoflurane is an inhaled general anesthetic. It is a highly fluorinated methyl isopropyl.
- This is often a well-tolerated general anesthetic for kids with autism.
- Because many anesthesiologists like to give Nitrous Oxide before administering Sevoflurane, please see the above information about Nitrous Oxide.
Versed
Versed is a benzodiazepine that causes relaxation and sleepiness. It also causes partial or complete memory loss.
- Versed tends to be a popular choice for sedating kids with autism.
- Precautions:
- Due to metabolic issues, some kids with autism do not get sleepy enough.
- Similarly, Versed can cause some people to go into a state of agitation, inconsolable hysteria, aggression, or restlessness instead of sedating them.
Conclusion
Due to common underlying health conditions, children with autism are more prone to regression post-anesthesia. However, it is possible to safely sedate your child for medical procedures, especially if you make the anesthesia team aware of your child’s diagnosis and the risks involved in sedating a child on the autism spectrum.
Additional Resources
The following is a list of studies, articles, and protocols to help you and your child’s medical team make an informed decision:
- Regression in Children with Autism Spectrum Disorder and Mitochondrial Dysfunction
- Guideline on Use of Nitrous Oxide for Pediatric Dental Patients
- Please note contraindications on page 2, which list:
- Methylenetetrahydrofolate reductase deficiency (MTHF)
- Cobalamin deficiency (B12)
- Please note contraindications on page 2, which list:
- Anesthetic Management of a Child with Unspecified Mitochondrial Disease in an Outpatient Dental Setting
- If you have a medically complex child, this paper might be helpful to the anesthesia team.
- Adverse Effect of Nitrous Oxide in a Child with 5,10 Methylenetetrahydrofolate Reductase Deficiency
- General Anesthesia and Methylenetetrahydrofolate Reductase Deficiency
- Mitochondrial Disease and Anesthesia
- Metabolic Precautions and ER Recommendations
- Anesthesia Protocol for Patients with Mitochondrial Disease (UT Mitochondrial Center of Excellence)