PANDAS/PANS and Autism

All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.

Nancy Hofreuter O’Hara, MD, MPH, FAAP
Pediatric Autoimmune Neuropsychiatric Disorders associated with Streptococcal Infections, or PANDAS, is a common autoimmune disorder with far-reaching movement, behavioral, and cognitive consequences. Although we focus on the pediatric population by definition with PANS and PANDAS, immune-mediated OCD/Tics/Neuropsychiatric Disorders can also affect adolescent and adult populations and should always be considered when specific signs and symptoms emerge. Both PANS and PANDAS are clinical diagnoses differentiated by the abrupt onset of symptoms as listed below.
As noted by Dr. Sue Swedo at the NIH in the late 1990’s, PANDAS involves antibodies from a streptococcal infection reacting with brain tissue (specifically the basal ganglia), triggering movement and behavioral problems. Rheumatic Fever is an older known disorder that illustrates this same disease process, in which antibodies from a streptococcal infection attack the heart valves, joints, and brain and result in heart disease, arthritis, and Sydenham’s Chorea. Although bacteria set the vicious cycle in motion, the real damage in this type of autoimmune disorder stems from the antibodies and the inappropriate immune response.
In 2012, the triggers for an abrupt onset of neuropsychiatric symptoms were expanded to include other infections such as Mycoplasma and viruses as well as metabolic disorders including exposure to pesticides or anesthesia. As such, in addition to PANDAS, we now utilize the acronym PANS, Pediatric Acute-Onset Neuropsychiatric Syndrome.
Diagnostic Criteria
- Abrupt, dramatic onset or recurrence of OCD
- Acute-onset anorexia and/or severe, restrictive eating disorder
- Concurrent presence of two of the following neuropsychiatric symptoms with severe and acute onset:
- Separation Anxiety
- Emotional lability
- Behavioral/developmental regression
- Sensory/motor abnormalities – handwriting deterioration
- Deterioration of school performance
- Urinary symptoms (urgency, frequency, enuresis)
- Sleep disturbance (difficulty falling asleep, REM disinhibition/restless sleep)
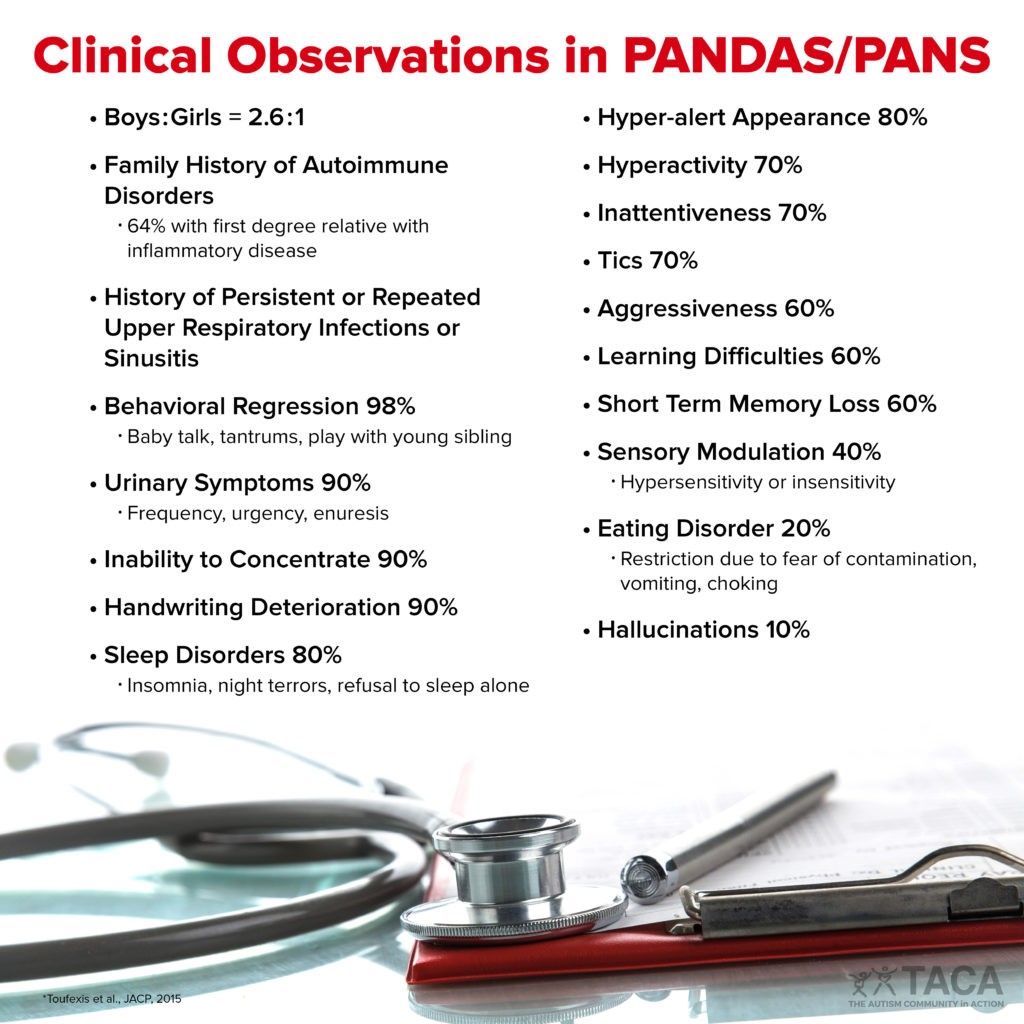
Additional Signs and Symptoms
There can be many signs, symptoms, and comorbid diagnoses noted in children with PANS/PANDAS including irritability, personality changes, aggression, uncontrolled agitation, fear about bedtime regimen, fidgetiness, emotional lability, motoric symptoms (tics, motoric hyperactivity, compulsive rituals), sensory defensiveness, impulsivity, depression, dysthymia, ADD, and ADHD in addition to those presented in the graphic below.
Testing
Always keep in mind that PANS and PANDAS are clinical diagnoses. Laboratory tools are limited and the traditional abnormalities of increased blood strep titers (ASO and DNAseB antibodies) and a positive throat culture are not always present. Therefore, normal levels of strep antibodies and negative cultures do not exclude the PANDAS diagnosis. Similarly, normal mycoplasma, viral or other titers do not rule out the diagnosis of PANS.
In atypical presentations, CaM kinase and anti-neuronal antibody testing can help to differentiate children with evidence of autoimmune encephalitis from those with tics, OCD, ADHD from other causes. The most commonly abnormal parameters (in > 56%) are immune markers such as ANA. Measuring other items such as zinc, magnesium, vitamin D and A and mitochondrial and thyroid markers may also be helpful in supporting appropriate treatments.
Treatment Options
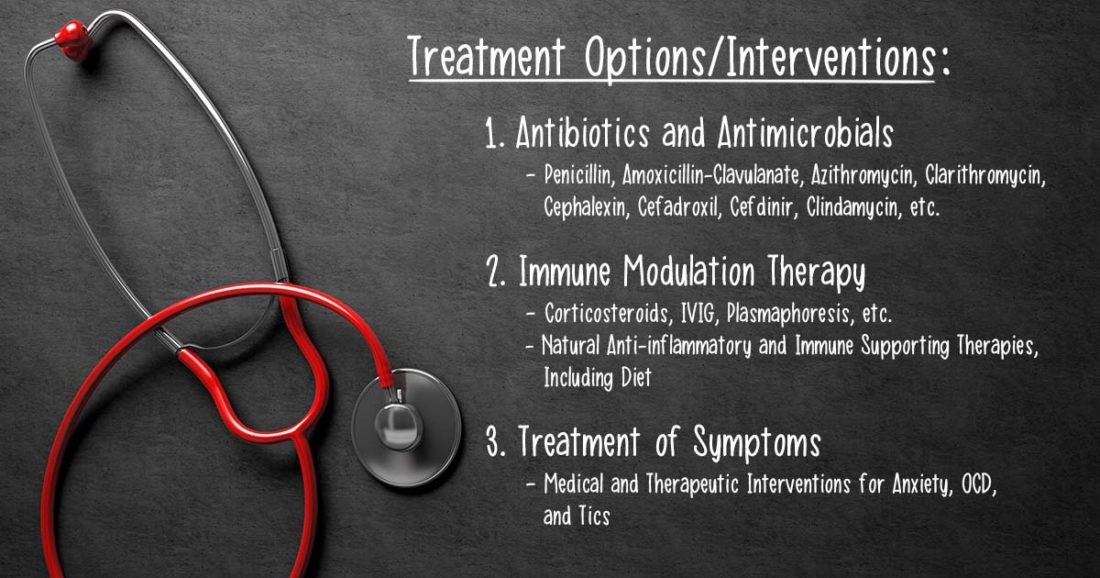
The treatment of children with PANS and PANDAS is three-fold including antibiotics/antimicrobials, comprehensive immune therapy, and treatment of symptoms.
1. Antibiotics and Antimicrobials
- Antibiotics
- Used daily for treatment; important to also consider prophylaxis to prevent further reinfection.
- Penicillin, Amoxicillin-Clavulanate, Azithromycin, Clarithromycin, Cephalexin, Cefadroxil, Cefdinir, Clindamycin, etc.
- Natural Antimicrobial Therapies
- Probiotics and Prebiotics including Saccharomyces Boulardii
- Xylitol and BlisK12 to treat germs in the mouth and nose
- Many herbs can help treat multiple germs:
- Antimicrobial herbs for strep including:
- Usnea
- Taiga (Pine needle extract)
- Berberine (Goldenseal)
- Neem
- Oregano Oil
- Cordyceps
- Antimicrobials herbs for mycoplasma:
- Berberine/Goldenseal
- Thyme/Oregano
- Colloidal Silver (also effective for strep)
- Houttuynia
- Antimicrobials to consider for viruses:
- L-Lysine
- Monolaurin
- Elderberry
- Olive Leaf
- Glycyrrhiza (Licorice)
- Lemon Balm
- Antimicrobial herbs for strep including:
2. Immune Modulation Therapy
- Corticosteroids
- Short-term use of tapering dose
- Positive response often indicates the patient is more likely to respond positively to IVIG, but no response does not mean IVIG will be ineffective
- Intravenous immunoglobulin (IVIG)
- Derived from human blood; pooled from many donors
- Can provide antibodies in those who are lacking them
- Can help to inactivate antigens and slow down an overactive immune system that is functioning inappropriately
- Plasmaphoresis
- A type of plasma transfusion to remove antibodies
- Intuximab
- Monoclonal antibody (off-label for lupus, MS, CIDP)
- Helminth Therapy
- HDCs, safe, and effective Primobiotics
Additional Considerations: Diet, Anti-Inflammatories, and Immune Modulators
First, diet is most important as food is medicine. A child’s diet needs to include whole foods, that are as organic and non-processed as possible. It should include foods high in antioxidants such as berries, artichokes, kale, spinach, beets, dandelion greens, red cabbage and dark chocolate. Use herbs and spices, particularly garlic, ginger, oregano, turmeric and cinnamon, adding little sprinkles to anything. Healthy oils include extra virgin olive, avocado and coconut oil. Meats should be grass-fed organic and wild-caught fish. Drink lots of water. Remove additives, sugars, gluten, casein, soy, and any food sensitivities as much as possible. Basically, this is an anti-inflammatory, healthy diet that all of us should be attempting to attain.
Additionally, a healthy treatment protocol includes anti-inflammatories and antioxidants as listed below:
- Anti-Inflammatories:
- Ibuprofen (10 mg/kg every 6-8 hours in the short term as needed for flares)
- Essential Fatty Acids–Omega 3 (EPA/DHA) and 6 (GLA)
- Aloe
- Curcumin
- Flavonoids – Quercetin, Luteolin, Rutin
- SPM
- CBD or Hemp Oil
- Antioxidants:
- Vitamin D, A, and C
- Zinc
- Resveratrol
- Melatonin
- N-acetyl Cysteine and Glutathione
3. Interventions To Consider for Treatment of Symptoms (Anxiety/ OCD/Tics)
Below, you will find interventions for treating symptoms associated with PANDAS and PANS, such as anxiety, OCD, and tics.
- Dietary Supplements:
- 5-HTP
- GABA
- L-Theanine
- Inositol
- Magnesium
- L-MTHF (if MTHFR mutation OR CFD)
- Ashwagandha
- Lemon Balm
- Motherwort
- Passionflower
- Mimosa Bark
- Hemp oil
- N acetyl Cysteine/Glutathione
- Exercise
- Meditation and mantras
Other Interventions to Consider for the Treatment of Symptoms
- Therapy
- CBT (Cognitive Behavioral Therapy) or DBT (Didactic Behavioral Therapy) can be particularly effective for children and families with PANS/PANDAS
- Removal of adenoids and tonsils
- Important intervention for those with recurrent strep or sleep apnea
- Also consider in certain cases where appropriate after discussing with your practitioner or referral to ENT familiar with PANDAS
- Treatment of yeast, parasites, clostridia as well as mold, lyme and co-infections as indicated by history and physical exam and as warranted
- Medications like SSRI’s (Prozac, Zoloft, etc) can often act as a “patch” for OCD or other symptoms
- However, they should only be considered for short-term use in certain cases and starting with very low doses, increasing slowly if needed
Conclusion
PANS/PANDAS is a devastating autoimmune disorder in children that highlights another link between chronic and recurrent infection and immune dysregulation and neuropsychiatric and behavioral problems. Most importantly, this is a clinical diagnosis of an abrupt onset of symptoms.
Ongoing clinical experience and emerging research reveals the depth and scope of problems stemming from PANS/PANDAS. While OCD and tics are still common, other issues like anxiety, bedtime fears or sleep issues, enuresis or other urinary symptoms, aggression, and deficits in learning, attention, and social interaction are among the many manifestations that result from PANS/PANDAS and impair the daily functioning and cognitive progress for many children.
Heightened clinical suspicion and more appropriate and comprehensive treatment with antibiotics/antimicrobials and immune-modulating therapy will transform PANDAS from a devastating chronic illness with episodic flares into a treatable disorder.
Additional Resources
Neuroimmune Foundation – A 501(c)(3) non-profit which advocates on behalf of individuals with neuroimmune and inflammatory brain conditions.
Aspire – A 501(c)(3) non-profit raising awareness about PANS/PANDAS while lending support to those affected by it.