Mast Cells and Autism

All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
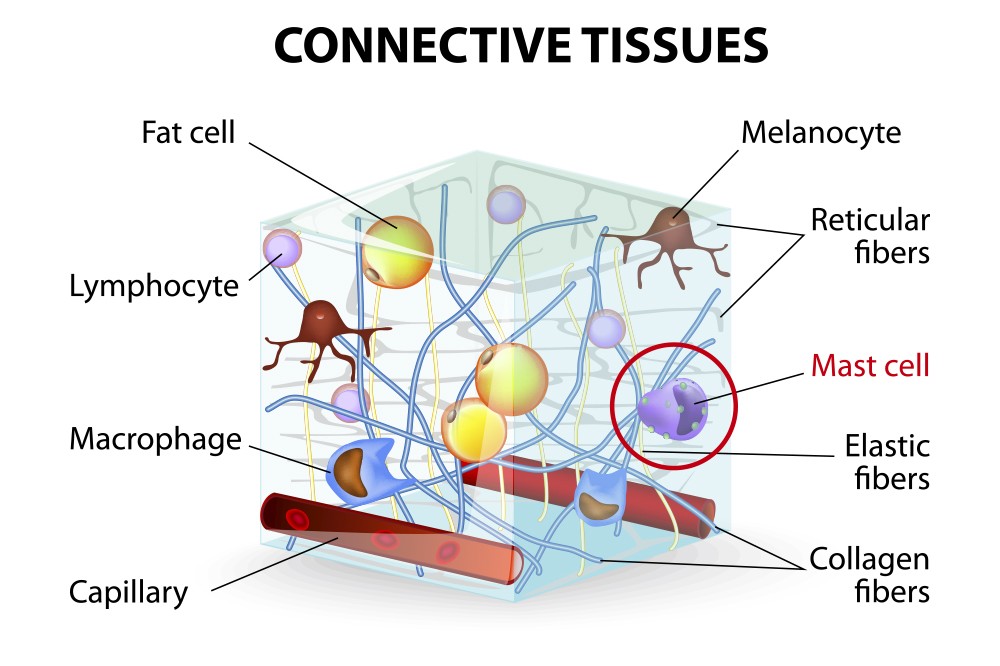
A mast cell is a type of white blood cell that is found in connective tissues all over the body, including under the skin, near blood and lymph vessels, and in the nerves, lungs, and intestines. We mainly think of mast cells when referring to something we are allergic to, but they do a lot more. Mast cells in the body are part of the immune system and orchestrate its responses.
Most importantly, mast cell disorders have increasingly been tied to autism.
This article includes:
- What are Mast Cell Disorders?
- Symptoms of Mast Cell Activation
- Mast Cells & The Blood Brain Barrier
- Treatment for Mast Cell Activation
- Removing triggers
- Supplements
- Medications
- Calming the immune response
- Diagnosing ATOPIC (allergic-like) Diseases
- Dark circles under the eyes
- Dermatographia
- Treat and observe for improvement
- Lab work
- Practitioners that can diagnose and treat mast cell activation
- Additional Resources
What are Mast Cell Disorders?
Mast cells are unique immune cells that are made in the bone marrow, travel briefly in the circulation as premature cells and mature into the tissues. Each mast cell contains about 500 secretory granules, each containing as many as 50 important biological mediators like histamine which is involved in allergic reactions.
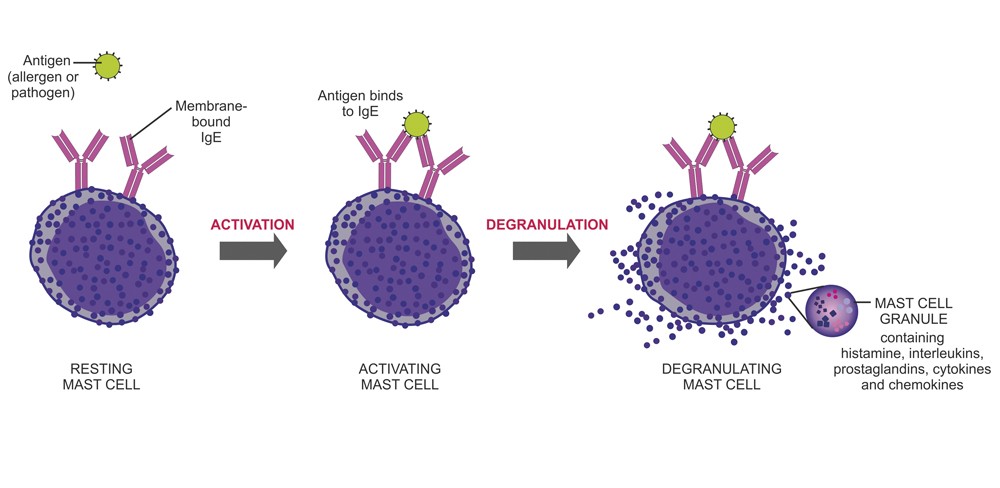
If a resting mast cell is stimulated by an allergic reaction, it will result in the mast cell “degranulating”, meaning the granules of the mast cell will release its contents of histamine, interleukins, platelet activating factor prostaglandins, proteoglycans, and enzymes such as tryptase. However, over the next 6-24 hours, other inflammatory molecules are released. In fact, it is now known that the mast cell can release inflammatory molecules without ever releasing histamine when exposed to neuroimmune triggers such as stress, hormones, and pathogens.
The photo below displays what happens when a stimulated mast cell degranulates.
Just as autism is a spectrum, so are mast cell disorders. They range from severe to mildly problematic but most of them are treatable.
Mast cell activation can fall into several categories:
- Primary mast cell activation
- This happens when too many mast cells are produced and spontaneously release their contents.
- This includes mastocytosis and is indicated by elevated serum tryptase.
- Secondary mast cell activation
- This happens when mast cells are activated by triggers such as food, medications, infections, or insect bites.
- It is characterized by hives, rashes, low blood pressure, and even anaphylaxis.
- Idiopathic Mast Cell Activation Syndrome (MCAS)
- There are strict criteria for this diagnosis.
- Includes repeated episodes of anaphylaxis along with other allergic symptoms such as hives, swelling, low blood pressure, and diarrhea.
- These episodes are associated with elevated tryptase, but the mast cell can release inflammatory molecules without releasing histamine or tryptase, such as prostaglandin D2 (PG2) and IL-6.
- Mast cell activation, unspecified
- This has a looser set of criteria.
- Gut problems are common with this diagnosis.
- Mast cells respond to odors, stress, and toxins but there is no tryptase released.
- Food intolerance
- This occurs when a person cannot digest a particular food or the food causes undesirable behaviors.
- Histamine intolerance
- This happens when the body produces too much histamine or cannot break down histamine in food.
- It is associated with low activity of the enzyme diamine oxidase (DAO).
Please note that these are all different diagnoses.
Disorders that involve mast cells
These are atopic (allergic-like) diseases and other disorders that involve mast cells:
- Allergies
- Asthma
- Eczema
- Food intolerance
- Eosinophilic Esophagitis
- Idiopathic urticaria
- Mastocytosis
- MCSS (multiple chemical sensitivity syndrome)
- Non-IgE food allergy
- Rhinitis
- Ehlers-Danlos Syndrome (EDS)
- Postural Orthostatic Hypotension (POTS)
- Chronic Inflammatory Response Syndrome (CIRS)
- Tick-Borne Illnesses (such as Lyme disease and co-infections)
- And now…. We can add autism to this list.
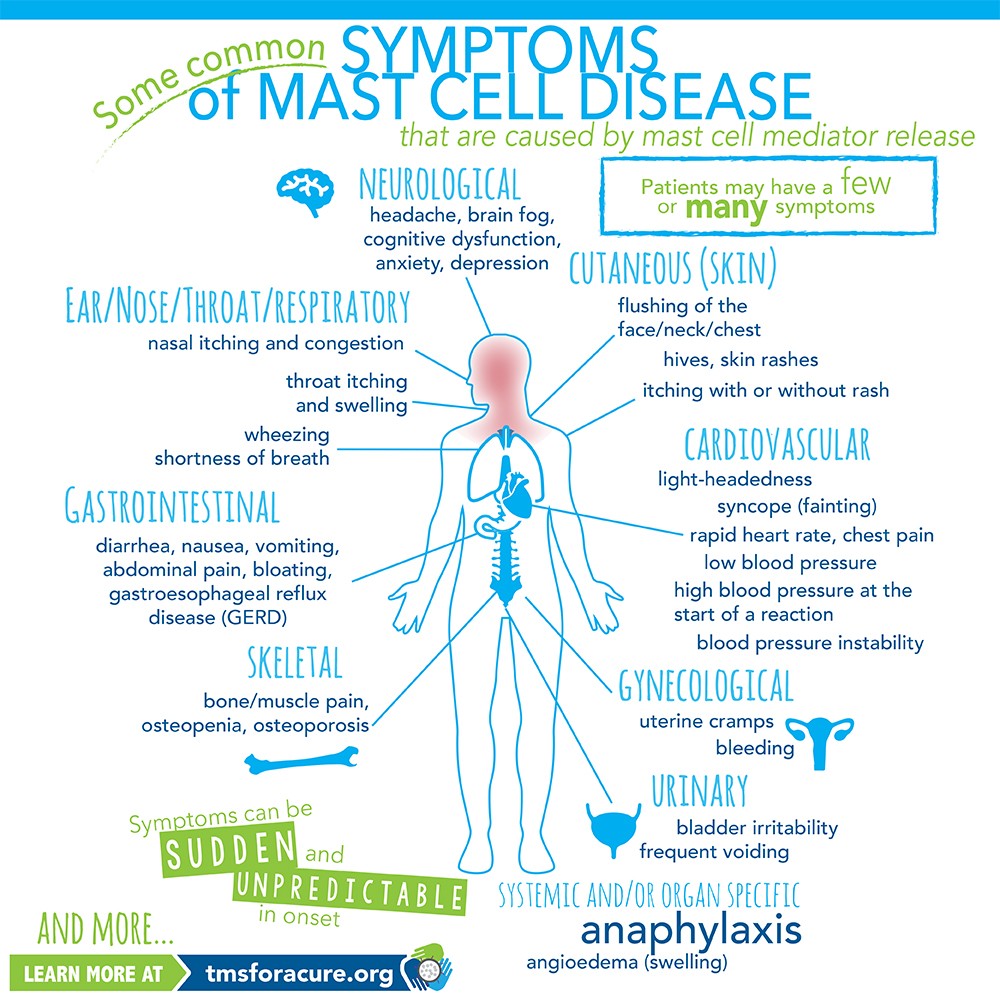
Symptoms of Mast Cell Activation
It is important to understand the symptoms of mast cell activation so you can identify it, in case your child experiences these difficulties. However, all these symptoms do not need to be present in mast cell disorders, and they may appear and disappear randomly.
- Diarrhea
- Flushing
- Headaches
- Brain Fog
- Hives
- Low blood pressure
- Itching
- Muscle pain
- Heart palpitations
- Shortness of breath
- Skin sensitivity to hygiene products or topicals
- Peripheral neuropathy (Numbness, tingling)
Mast Cells & the Blood Brain Barrier (BBB)
The brain does not have immune cells that fight infection. Instead, it has microglia that regulate immunity in the brain. Mast cells surround the blood brain barrier, which protects the brain against toxins and pathogens. Therefore, that makes mast cells the brain gatekeepers. They control the blood brain barrier that allow molecules into the brain that activate the microglia. When microglia increase, we see inflammation in the brain. Interestingly, increased microglia have been found in the brains of post mortem people diagnosed with autism. In addition, the mast cells can release molecules which themselves can activate microglia and then the microglia release pro-inflammatory mediators.
In other words, activated mast cells can increase blood brain barrier permeability, which leads to inflammation of the brain and autism.
Treatment for Mast Cell Activation
Treatment for mast cell activation involves limiting triggers that cause mast cell degranulation, stabilizing mast cells, and inhibiting the action of some mediators after they are released (such as histamine, leukotrienes, etc.)
Removing Triggers
The top intervention for mast cell activation will always be identifying and removing triggers from your body, your diet, and your environment. Everyone’s triggers are different. Unfortunately, there are no tests to determine your child’s mast cell triggers. Therefore, it will require some detective work.

Possible triggers that need to be considered are:
- Gluten
- Casein
- Environmental allergens
- Perfumes (including essential oils)
- Electromagnetic waves (EMFs)
- Flame retardants
- Heat and/or cold
- Plastic
- Polyethylene glycol (PEG)
- Stress
- Mold
- Viruses and bacteria
- Glyphosate
- Heavy metals
- Artificial Colorings
- Preservatives
- High histamine foods such as fermented foods, smoked meat, cheese, avocado, tomato, and spices. Find a list here*.
- Foods high in salicylates*
- Highly allergenic foods*
*Please note: ANY food can be a trigger to your child. You will likely have to do an elimination diet to conclude what foods are problematic.
Supplements to treat mast cell activation
There are supplements that have many benefits including stabilizing mast cells, breaking down histamine, modulating the immune system, and reducing inflammation. Therefore, using specific supplements may lead to an improvement in symptoms.

Supplements that inhibit mast cells:
- Quercetin
- Inhibits the release of histamine, prostaglandins and leukotrienes, but is high in phenols.
- Less than 10% is absorbed in powder form
- Luteolin
- Inhibits mast cells activation & less phenolic than quercetin
- Enters the brain
- Vitamin D
- Make sure to test blood levels of Vitamin D3 (1, 25-OH)
- Anti-inflammatory
- Rutin
- Inhibits histamine release after broken down in the gut
Supplements that support the immune system:
- Curcumin
- Inhibits the degranulation of mast cells but it also decreases DAO
- Zinc
- Inhibits allergic responses
- Vitamin C
- Increases DAO to break down histamine.
- Vitamin E
- Inhibits histamine release
Supplements that are antioxidants
- Resveratrol
- Inhibits IgE allergy reactions
- Very high phenol content
- Green Tea (EGCG)
- Anti-allergic
- Pycnogenol
- Antioxidant; inhibits histamine release
Supplements that are anti-anxiety
- Magnesium
- Deficiency leads to increased mast cells
- Ashwagandha
- May help with stress and anxiety
Supplements that metabolize histamine
- DAO (Diamine Oxidase Enzymes)
- Breaks down histamine
- Vitamin B6
- Enables DAO to break down histamine
- Bifido infantis and Lactobacillus rhamnosus
- Probiotics that are histamine degrading
Supplements that support brain function
- Calcium folinate
- Pushes folate into the brain to support cognition
Please note the following:
- Children prone to mast cell activation can be very sensitive to supplements. Therefore, the quality of supplements chosen is very important. They should be greater than 95% pure and free of casein, gluten, lactose, dyes, PEG, and other additives.
- If your child has a slow functioning COMT enzyme (shown as COMT++), they cannot break down adrenaline (epinephrine) and dopamine well. Hence, they may have trouble processing catechols. Both quercetin and green tea extract are very high in catechols. Therefore, people that are COMT homozygous may experience increased anxiety and other undesirable effects when taking them.
- In addition, most supplements that help with histamine are high in phenols. If your child is sensitive to phenols (such as chocolate or berries), you have to be very careful about what supplements are chosen for your child. You can find symptoms of phenol sensitivity in the TACA article on Phenols, Salicylates, and Additives.
Medications commonly used to treat Mast Cell Activation
There are numerous medications used to treat mast cell activation depending on the patient’s symptoms.

Medications:
- Histamine 1 blockers
- Hydroxyzine (Atarax)
- This is also an anti-anxiety medication
- Doxepin (Silenor)
- Cyproheptadine (Periactin)
- This is also antiserotonergic; good for gut problems and headaches
- Loratadine (Claritin)
- Fexofenadine (Allegra)
- Diphenhydramine (Benadryl)
- Avoid red colored pills. Use clear gel caps.
- Cetirizine (Zyrtec)
- Hydroxyzine (Atarax)
- Histamine 2 blockers
- Famotidine (Pepcid, Pepcid AC)
- Mast Cell Stabilizers
- Cromolyn
- Cromolyn Sodium, Gastrocom—oral form
- It is a weak mast cell inhibitor. Less than 5% absorbed in the gut. The body gets used to it very quickly.
- Nasalcrom—nasal spray
- Opticrom—eye drops
- Cromolyn Sodium, Gastrocom—oral form
- Ketotifen (weak mast cell stabilizer and an H1 blocker)
- Zaditor – eye drops
- Cromolyn
- Leukotriene blockers
- Montelukast (Singulair)
- Useful with asthma
- Zafirlukast (Accolate)
- Zileuton (Zyflo)
- Montelukast (Singulair)
- Antibody neutralizer
- Omalizumab (Xolair)
- This is injectable.
- It is approved for ages 4 years old and over, for chronic asthma and chronic urticaria (itching).
- Omalizumab (Xolair)
Other Treatments Unrelated To Mast Cells For Consideration
Calming the immune response
While these interventions are unrelated to mast cells, they may still help your child. In addition to supplements and medication, many people find success by calming the immune response with immune modulation.
Please keep in mind that people with mast cell activation problems tend to be very sensitive, so if you use LDN, LDA, or homeopathy, please find a practitioner familiar with treating mast cell disorders, and introduce it slowly and in very low doses.
Low-dose Naltrexone (LDN)
Many parents tell us they are finding relief using LDN for mast cell activation. LDN is a prescription competitive opioid receptor antagonist drug. When naltrexone is given in very low doses (<1 mg/day), it may reduce inflammation, pain, and help modulate the immune system. It is typically introduced in step-up dosing at night.
Low-dose allergen (LDA) immunotherapy
This approach is used to desensitize the body mostly to environmental and food allergens. Please be sure to use certified practitioners to oversee this approach.
Homeopathy
Homeopathy is the theory of “like treats like”. It is based on the idea that substances that produce symptoms of sickness in healthy people will have a healing effect when you give very dilute quantities to sick people who exhibit those same symptoms. By triggering the body’s own healing processes, this approach restores homeostasis. Again, please make sure your practitioner is familiar with mast cell activation and knows to dose very low and slowly.
Mindfulness/Meditation
Stress exacerbates mast cell activation. Therefore, reducing stress has a profound effect on calming mast cells and the immune system. Meditation and mindfulness to quiet the mind can have an overwhelmingly positive effect on the body. This can be a difficult practice to teach children but incorporating yoga, breathing exercises, and a positive outlook can all make a huge difference.
Diagnosing ATOPIC (Allergic-Like) Diseases
The next thing we will address is how to diagnose mast cell activation conditions. Below we have listed some red flags to look for and the lab work that is typically run with a specialist.
Dark circles around the eyes
Look for dark circles under your child’s eyes. We refer to these as “allergy shiners”. Although mast cells are not the only reason for dark circles around the eyes, most of the time people with them respond to mast cell treatment.

Dermatographia
Dermatographia (writing on the skin) is another hint that mast cells are overactive. This occurs when mast cells in the skin respond to pressure. If you scratch the surface of the skin with a dull object, does the skin become raised and red after a few minutes? See image below for an example.

Treat and look for improvement
Finally, the easiest way to check for a mast cell disorder is to treat it, then look for improvement in overall symptoms.
Lab work
However, some lab work would be useful. Testing for mast cell disorders typically involves the following tests.
Labs:
- IgE, IgA and IgG (and IgG subclasses 1 & 4)
- Anti-IgE receptor antibody (basophil activation)
- Heparin
- IL-8 (a pro-inflammatory cytokine)
- IgE (RAST) testing for at least:
- alpha gal
- dairy (casein, lactoglobulin)
- wheat (gluten)
- dust mites
- fungi (molds)
- grass
- pollen
- animal dander
- IL-4, IL-6 (pro-inflammatory cytokines)
- Prostaglandin -D2
- Tryptase (best to test while having a reaction for most accurate results)
- 24-hour Urine Histamine
- Must be collected and sent to the lab cold
- Methylhistamine or MIA
- Must be collected and sent to the lab cold
- 23BPG=2, 3-Dinor-11 (beta)-PGF (2a)
- Must be collected and sent to the lab cold
- Prostaglandin D2 (PGD2)
- Must be collected and sent to the lab cold
- Heavy Metals (in urine)
- Mycotoxins (in urine)
Practitioners that can Diagnose and Treat Mast Cell Activation Disorders
Now that you have this information, you are probably wondering what type of doctor can diagnose and treat mast cell activation.
If your child is having gastrointestinal issues, you need a specialty gastroenterologist and allergy team. Your child may be suffering from eosinophilic esophagitis, intestinal mastocytosis, or eosinophilic gastroenteritis. It is important to evaluate stool for histamine, calprotectin, and eosinophilic cationic protein. You can find a listing of qualified GI doctors at APFED.
Typically, the doctors that are best equipped to diagnose your child with a mast cell disorder are specially trained allergists or hematologists/oncologists. The best way to find one for your child, is to ask for local recommendations in one of the many specialized mast cell Facebook groups. You want a group familiar with mast cell activation disorders, not simply mastocytosis. A good example is the Mast Cell Society Facebook Group.
Functional medicine doctors are fabulous for pulling together the pieces of the puzzle and they should be able to trial your child on supplements or medications that may help. However, they likely do not have the training necessary to assess which mast cell disease is present, or do a differential diagnosis that will rule out other conditions that present like mast cell disorders. This is why adding a specialist to your child’s medical team should be a consideration if your child has symptoms.
Lastly, while allergists can determine IgE allergens and it is important to know what those are, it is equally critical to remember that allergy testing will not identify all mast cell triggers or sensitivites. Finding your child’s triggers is not always something a doctor can help you with. You may need to do this at home with an elimination and challenge diet, as was mentioned above in the treatment section.
Be Prepared when Seeing your Doctor
Whatever specialist you chose, make sure to bring documentation of your child’s reactions and behaviors. Keep a journal, take pictures of rashes, video behaviors, and always bring previous lab work. This will allow the doctor to get an accurate picture of what you are seeing and why you are considering a mast cell activation disorder as a possible diagnosis.
Conclusion
Many epidemiological studies have shown a strong association between autism and mast cell disorders. Numerous people on the autism spectrum experience mast cell activation which manifest as differing symptoms. Treating mast cell activation can bring about improvements in core autism symptoms.
Additional Resources with Information About Mast Cell Activation
Mast Cell Activation Disorder: A Primer for the Gastroenterologist (2020)
Is a subtype of autism an allergy of the brain? (2013)
Brain mast cells link the immune system to anxiety-like behavior (2008)
Mast Cell Research by Dr. Theoharides at Tufts University
Mast Cells, Stress, Fear and The Autism Spectrum Disorder (2019)
Atopic diseases and inflammation of the brain in the pathogenesis of autism spectrum disorders (2016)
Ways to Address Perinatal Mast Cell Activation and Focal Brain Inflammation, including Response to SARS-CoV-2, in Autism Spectrum Disorder (2021)
Luteolin supplements: All that glitters is not gold (2021)
The Mast Cell Disease Society, Inc.
Mast Cell Activation Syndrome: Proposed Diagnostic Criteria (2010)
Mast Cells: The immune gate to the brain (1990)
Contributing Editor
Theoharis Theoharides, BA, MS, MPhil, PhD, MD, FAAAAI
Dr. Theoharides is Professor of Pharmacology and Internal Medicine, as well as Director of Molecular Immunopharmacology and Drug Discovery, in the Department of Immunology at Tufts University School of Medicine. He first showed that mast cells, known for causing allergic reactions, are critical for inflammation, especially in the brain, and are involved in a number of inflammatory conditions that worsen with stress such as allergies, asthma, autism spectrum disorder, eczema, fibromyalgia, interstitial cystitis/bladder pain syndrome, mast cell activation syndrome, migraines, multiple sclerosis, myalgic encephalomyelitis/ chronic fatigue syndrome and psoriasis. Dr. Theoharides is also the Scientific Director of Algonot, LLC