The Gut-Brain Connection
All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
There is good reason the gut is referred to as a person’s second brain. Over 70% of our immune system resides in the gut. Additionally, recent studies show that the metabolites produced by the gut microbiota include neurotransmitters such as glutamate, GABA, serotonin, and dopamine. Therefore, the gut influences our mood as well as protects us against infection.
However, up to 70% of children with autism have impaired GI function. In turn, this directly affects brain function.
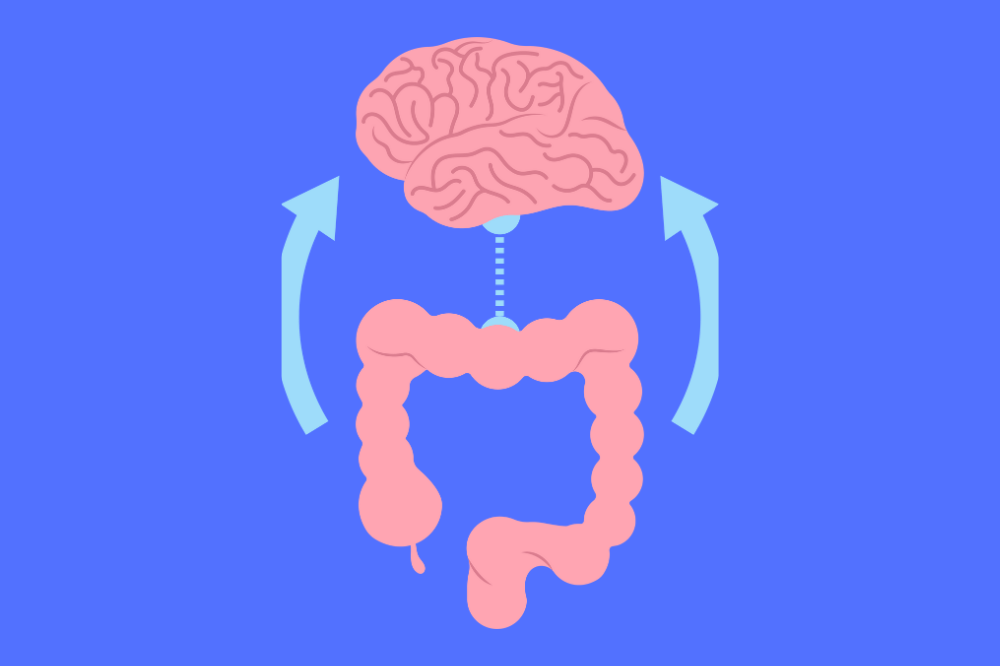
The central nervous system (CNS), consisting of the brain and spinal cord, and the gastrointestinal system have a two-way communication network of signaling pathways that make up the gut-brain axis.
Research continues to demonstrate differences in vagal tone, the immune system, and the microbiome (bacteria, parasites, fungi and viral flora in the intestines) in individuals with autism. Consequently, this information shows the complex connections between the brain and the gut and is also is providing new insights into treatments for autism.
This article will discuss:
- The connection between the gut and the brain
- Key regulators of the gut–brain connection
- Treatments to improve gut–brain connection
What is the Gut-Brain Axis?
The gut-brain axis refers to the two-way communication system between the digestive system and the nervous system. Research has only begun to fully understand the complexities of this communication system and its impact on our mood, behavior, digestion, and ability to learn and process information. In fact, researchers have discovered that within the walls of the digestive system is the enteric nervous system (ENS), or “second brain” which contains more neurons than in either the spinal cord or the peripheral nervous system. This second brain in the digestive tract is in constant communication with the brain.
Examples of communication between the gut and brain:
- The brain manages gut function through the hypothalamic-pituitary-adrenal axis (HPA axis) and the autonomic nervous system. (The autonomic system regulates involuntary processes such as heart rate, blood pressure, breathing, and digestion.)
- The gut impacts the central nervous system (CNS) function through the involvement of microbial (bacteria/yeast/viruses) by-products and gut hormones that travel through the enteric nervous system (ENS), vagus nerve, circulatory system, or immune system to reach the brain.
Key Regulators of the Gut-Brain Axis
The key factors contributing to a healthy gut – brain connection are a diverse gut microbiome, tight junctions in the gut lining, and a well-toned vagus nerve. We will discuss each below.
Gut Microbiota
The gut microbiota are the thousands of microorganisms including bacteria, fungi, and viruses, that live in our digestive tract. The signaling pathways involved in the gut-brain axis are impacted by these microorganisms and what they produce. Indeed, the gut microbiota has been demonstrated in studies as having a role in many conditions including autism, anxiety, obesity, schizophrenia, Parkinson’s disease, and Alzheimer’s disease.
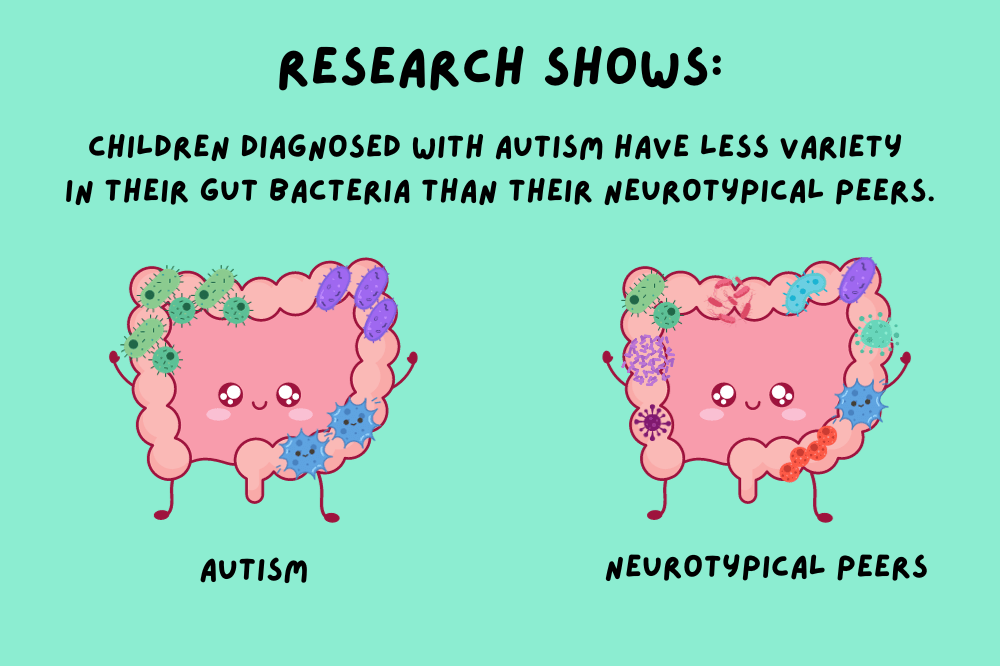
Interestingly, studies tell us that there is a lower microbial diversity found in the guts of children with autism compared to their neurotypical peers. (1)(2)(3)(4)(5)
The high prevalence of GI dysfunction in autism and its connection to challenging behaviors and symptoms suggest the relationship between gut and brain dysfunction in a significant subset of individuals with autism. Moreover, increasing evidence suggests that one of the key modulators of gut-brain communication is the intestinal microbiome.
Many factors impact the microbiota composition in early life such as infection, birth/delivery, antibiotic use, nutrition, environmental stressors, and genetics. Specifically, Harvard & MIT researchers have linked maternal immune activation (MIA) to autism and have shown that maternal infection during pregnancy can alter the microbiome and impact brain development.
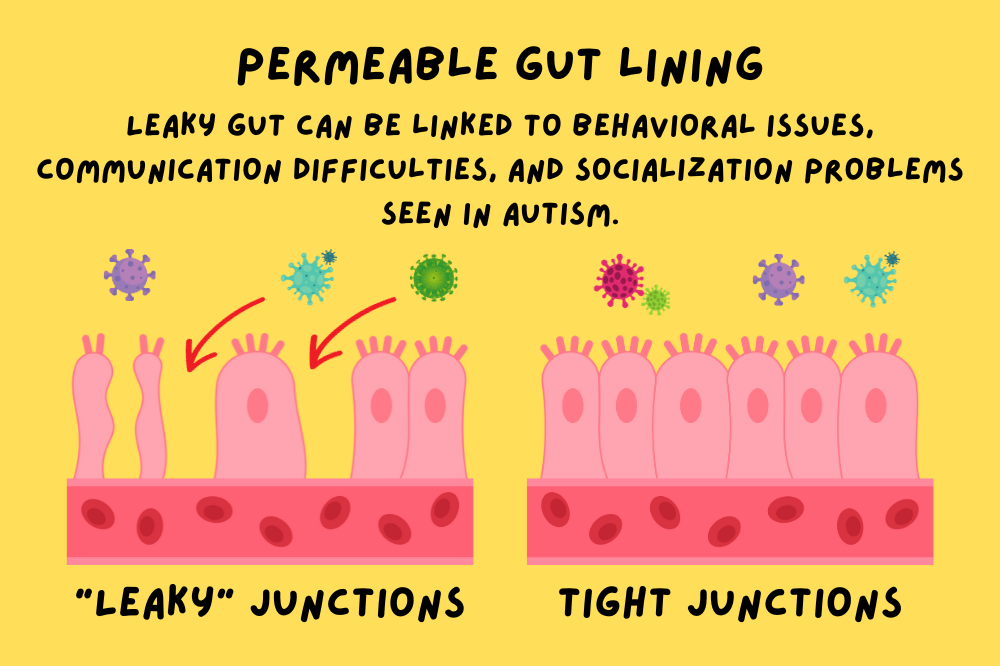
Gut Permeability and the Blood Brain Barrier
Gut permeability refers to an unhealthy gut lining where the junctions are not tight enough, allowing partially digested food particles, toxins, and bacteria to gain access to the bloodstream. We call this “leaky gut”. In mice studies, a leaky gut was shown to dysregulate gene networks in the brain associated with immune activation, oxidative stress, and myelination. Therefore, what is happening in the gut can affect the behaviors we see in autism. Additionally, biomarkers of leaky gut are being investigated as possible diagnostic tools for autism.
Factors that contribute to gut permeability (leaky gut) are:
- Stress
- Zonulin (in gluten)
- Mast cell degranulation
- Glyphosate
- Imbalances in the microbiota (also known as dysbiosis)
These can also lead to permeability of the Blood Brain Barrier (BBB).
Many Individuals with autism have increased challenges with yeast and bacterial overgrowth. For example, results from this 2018 study show that anti-Candida albicans antibodies were found in 36.5% of children with autism versus only 14.3% in neurotypical kids. With dysbiosis (yeast/bacterial imbalance in the gut), the signaling pathways involved in the gut-brain axis are dysregulated and associated with altered permeability of the blood-brain barrier (BBB) and brain inflammation.
Some doctors may run an IgG food sensitivity test. However, if the test comes back with numerous food sensitivities, it is simply a sign that there is a leaky gut barrier allowing food particles into the bloodstream where the body makes antibodies against that food. The solution is healing and sealing the gut. (See the treatment section of this article.)
Vagus Nerve
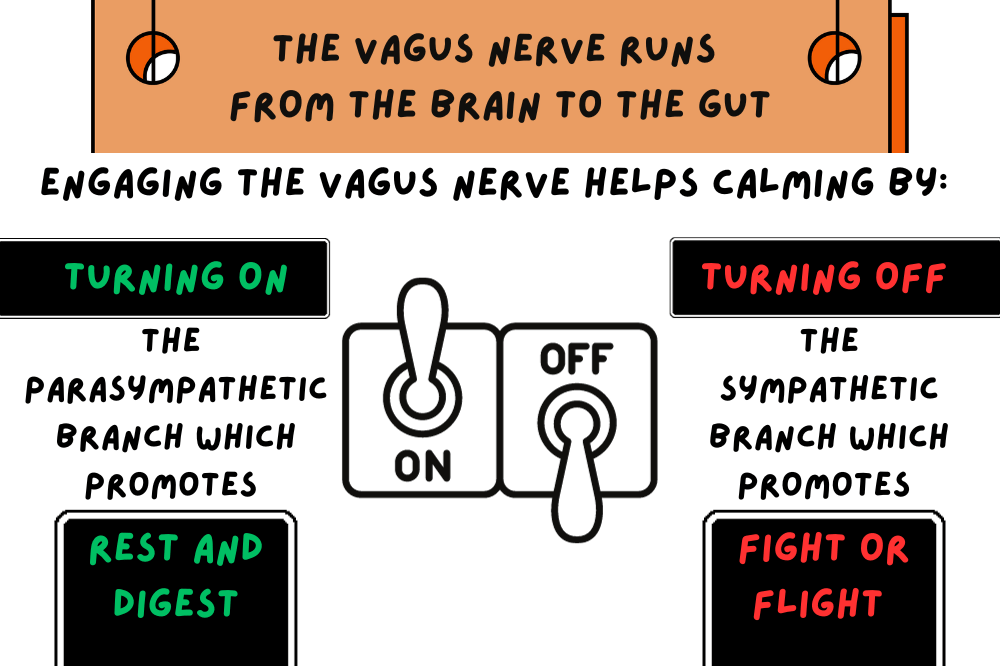
The vagus nerve is the longest nerve in the body and connects the brain to various organ systems in the body including the gut. Moreover, the vagus nerve is a contributing part of the autonomic nervous system (ANS). The ANS works “automatically” to regulate vital functions in the body such as breathing, heart rate and digestion.
There are two parts to the autonomic nervous system:
- Sympathetic Nervous System: Prepares the body for “fight or flight”.
- Parasympathetic Nervous System: Returns the body to a calm state (“rest and digest”).
The fight or flight response occurs as the amygdala in the brain responds to stress. In autism, stress and environmental triggers stimulate mast cells and microglia causing dysfunctional neuronal connectivity. This process can lead to an exaggerated “fight or flight” reaction.
The vagus nerve helps to disengage the sympathetic nervous system fight/flight response. Furthermore, low vagal tone results in challenges with the vagus nerve fluidly adapting between the sympathetic and parasympathetic and helping to return the body from an exaggerated fight or flight reaction to a calmer state.
Increasing your vagal tone activates the parasympathetic nervous system. Additionally, stimulating the parasympathetic nervous system can:
- Decrease Inflammation
- Help kids that are picky eaters or have trouble swallowing
- Aid in digestion
- Help anxiety
- Help control PANS symptoms
Some doctors are even using implanted vagus nerve stimulators to control epilepsy.
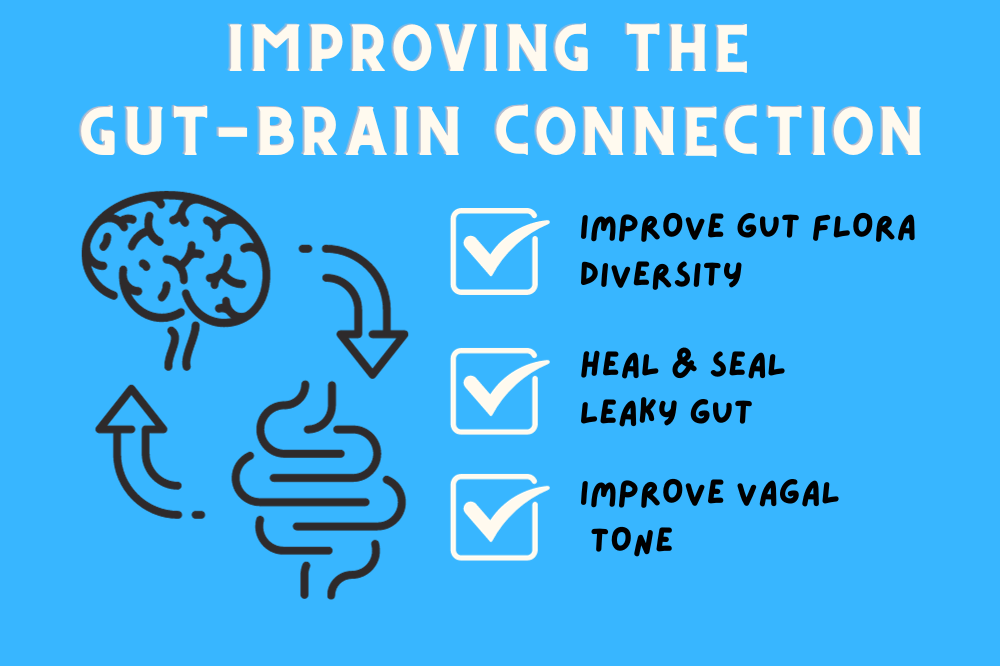
How to improve the Gut-Brain Connection
All this leads us to the big question: How do I improve my child’s gut-brain connection? This section will review diversifying gut flora, healing and sealing leaky gut, and improving vagal tone.
Improve Microbial Diversity
It is important to have a wide variety of bacteria in the gut. In order to accomplish this, work on improving diet, adding bacteria, and looking ahead to the research on fecal matter transplants for autism.
Diet:
By far, the most effective way to improve microbial diversity is to eat a wide variety of whole foods. Note that eating the same thing every day only works to encourage the same bacteria growth. Trying new foods and rotating foods both feed different bacteria in the gut.
Probiotics, prebiotic foods, and vegetable ferments:
Use prebiotics or probiotics depending on Ombre stool testing & OAT results:
- Too much Bacteroides, Allistipes, parabacteroides, Prevotella indicates a need for:
- High fiber diet
- No inulin
- Not enough Bacteroides, Allistipes, parabacteroides, Prevotella indicates a need for:
- Inulin (short-term only)
- Animal based protein
- S. Boulardii
- Too much Bacillus, Clostridium, Enterococcus, Lactobacillus, Ruminoccocus indicates a need for:
- Lactulose
- High Bifido requires berberine
- High Clostridia (on OAT) requires Carnitine, S. Boulardii, High dose probiotics
- Not enough Bacillus, Clostridium, Enterococcus, Lactobacillus, Ruminoccocus indicates a need for:
- Inulin
- Plant based diet
- Resistant starches
- Lactobacillus Rhamnosus (gg)
- Bifido Logum
Fecal Matter Transplant (FMT):
Researchers Dr. James Adams and Dr. Rosa Brown have trialed a special kind of fecal matter transplant called Microbiota Transplant Therapy (MTT) that is demonstrating improvements in kids with autism. This is still in trial phases and is not yet approved to treat autism. You can read more about it below:
- ASU researchers use bacteria to improve autism symptoms – Arizona PBS (azpbs.org)
- Shotgun Metagenomics Study Suggests Alteration in Sulfur Metabolism and Oxidative Stress in Children with Autism and Improvement after Microbiota Transfer Therapy – PubMed (nih.gov)
Heal and Seal Leaky Gut
The process of healing leaky gut is often referred to as “The 4 Rs” – Remove, Replace, Repair, Reinoculate. Therefore, there are numerous steps and ingredients to help tighten cell junctions.
REMOVE Inflammatory triggers, such as:
- Processed foods
- Gluten, Dairy, and Soy
- Other foods that your child may be reacting to
- Refined and unrefined sugar
REPLACE inflammatory triggers with:
- Omega 3 fatty acids (fish oil)
- Nourishing, whole foods
- Fiber-rich foods
- Psyllium husk, vegetables and fruit
- Healthy protein
- Lean meat, Nuts and seeds, and fish
Sometimes this stage will also require digestive enzymes when the body has trouble breaking down food and absorbing nutrients. Protease to digest proteins, lipase to help digest fats and amylase to help digest carbohydrates.
REPAIR the gut with:
- L-Glutamine
- Slippery Elm
- Aloe
- Zinc Carnosine
- Butyrate
- Mitochondrial support to help gut motility
There are some combination GI repair products that include these ingredients and more. However, if your child does not tolerate the supplement, it is difficult to know the culprit. You might consider trying one ingredient at a time.
If you skip this step and go straight to probiotics, you may find your child responds poorly with aggression, irritability, or even autoimmune issues. In addition, there may be other issues at play such as small intestine bacterial overgrowth (SIBO) causing a poor response to probiotics.
REINOCULATE the gut with:
- Probiotics
- Fermented foods
- Prebiotics
Remember that probiotics are simply a handful of bacteria strains added to the gut. The human gastrointestinal microbiota contains approximately 300 to 500 bacterial species with nearly 8000 strains of bacteria. Taking only a handful of strains can skew the gut microbiome, so many doctors advise only taking probiotics for short periods of time and changing strains often. Additionally, different strains of bacteria have different functions.
Fermented foods (if tolerated) such as yogurt, kefir, uncooked sauerkraut, and kimchi contain many more strains of bacteria than probiotics. Therefore, they tend to be a better option. Always start very slowly with fermented foods and watch for reactions. They can be extremely strong.
By contrast, prebiotics are a food source for your existing gut bacteria. They are found in both fruits and vegetables and in supplements (such as inulin and fructooligosaccharides). Fermentation of prebiotics by gut microbiota produces short-chain fatty acids (SCFAs) which are important to the health of the colon. Since they feed what is already living in the gut, you need to be careful not to feed existing pathogenic (bad) bacteria. If you do, it can overgrow and cause worsening of symptoms. Doing a stool test (as is outlined in this TACA article on lab testing) can tell you if there are pathogenic bacteria that you need to be aware of.
Improve Vagal Tone
Ways to improve vagal tone are listed below:
- Cold exposure. Turning the water temperature to cold in the last 30 seconds of a shower can reduce sympathetic activation over time.
- Deep belly breathing. Slow inhaling through your nose making your stomach expand outward. Your exhale should be long and slow through the mouth.
- Safe and Sound Protocol: This is a listening system based upon Dr. Stephen Porges’ Polyvagal Theory.
- Singing, chanting, humming, gargling: The vagus nerve is connected to your vocal chords and muscles at the back of the throat.
- Heart Rate Variability (HRV) Biofeedback. Read more about it in this TACA article on Autism Treatment Methods.
Conclusion
As you can see, gut health directly impacts brain health. And likewise, the brain manages gut function through the autonomic nervous system. Improving microbial diversity in the gut, healing and sealing permeable intestines, and improving vagal tone will all ultimately help brain function in our children.
Additional Research
- The Brain-Gut-Microbiome System: Pathways and Implications for Autism Spectrum Disorder – PMC (nih.gov) (Check out the great graphic)