Sleep Issues in ASD

All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
Studies show that 53% percent of children with autism have at least one frequent sleep problem. Unfortunately, typical treatments are often short-lived as they don’t always deal with the underlying cause of the sleep issue. In this article, we will provide some tips to help improve your child’s sleep and discuss common medical causes of sleep issues in autism.
Sleep issues not only impact your child’s behavior and health, but are also associated with cognitive, verbal, and attention impairments. So, as you can see, ensuring that your child obtains an adequate amount of sleep can enhance their quality of life.
Tips to Help Alleviate Sleep Issues
Before we discuss the medical causes of sleep issues in autism, let’s talk about some simple things you can do at home to help your child sleep. Below is a list of tried-and-true tips that can help the whole family get more Zzz’s.
Epsom Salt Baths
½ cup to 1 cup of Epsom salts in a warm bathtub can be calming for many children. You may even want to try adding a drop or two of lavender essential oil to their bath (lots of parents swear by it).
Eliminate Electronic Use One Hour Before Bedtime
Studies show a significant relationship between increased screen time and sleep disturbances. Children who use electronics before bedtime are more likely to have a difficult time falling asleep, have trouble staying asleep, and get less overall sleep than children who do not watch TV or use electronic devices before bed.
A Set Routine
Routine can be very important for kids, but especially kids with autism. A calming bedtime routine including quiet music or a metronome, weighted blankets, a darkened room, massages, Epsom salts baths, and avoiding TV or stimulating toys/music can set the stage for a good night’s sleep. Consider using a visual schedule and set nighttime expectations to lessen bedtime anxiety.
Limit EMF Exposure
Just like light, exposure to electromagnetic fields (EMFs) can also interfere with the body’s melatonin levels. Limit your child’s EMF exposure by turning off your Wi-Fi router, unplugging cordless phones, and powering down all computers, tablets, and smart phones each night before bed. Learn more about EMFs and what you can do to limit your child’s exposure to them here.
Exercise
Make sure your child is getting some form of exercise each day. The bulk of the research out there indicates that exercise can help boost sleep duration in addition to sleep quality (regardless of the mode and intensity of activity). Pick a fun activity to do together or go for a walk, and don’t forget to add an extra glass or two of water throughout the day to ensure your child is adequately hydrated.
Medical Causes of Sleep Issues in Autism
If you have tried all of the above and your child is still having trouble with sleep, please consider asking your child’s doctor to evaluate if an underlying medical issue is causing your child’s sleep issues.
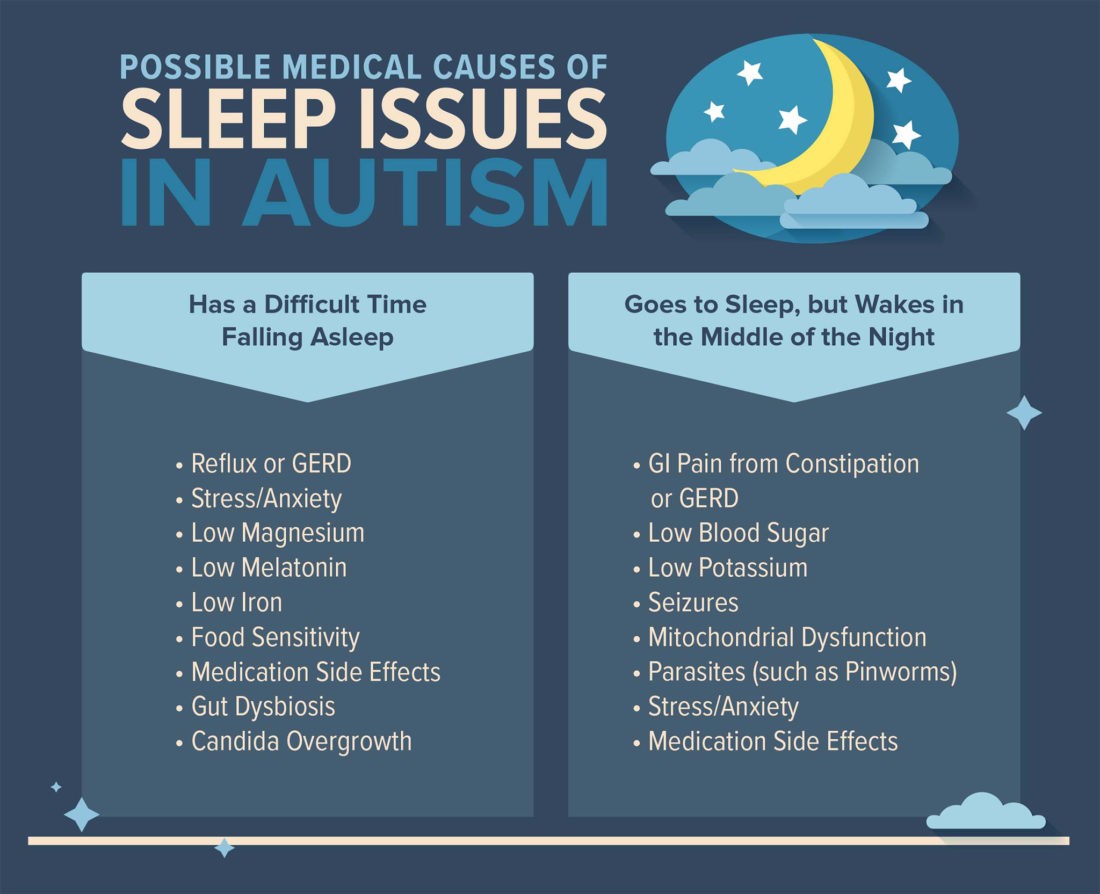
Low Potassium
If your child has trouble staying asleep, they could be low in potassium. Read more about low potassium and its relationship to sleep disturbances here.
Iron Deficiency
A full iron panel plus ferritin can check for low iron. Vitamin C can help the body absorb iron. Please note that high levels of iron can be toxic in children, so it is important to only supplement iron under the direction of your child’s physician. Studies showing a relationship between low iron and sleep issues in autism can be found here and here.
Constipation
The pain alone is enough to wake the child during the night. Look for posturing, lack of appetite, loose stools (which are indicative of a blockage), not eliminating completely, and more. The best way to check for constipation is with a KUB, which is an abdominal x-ray. Talk to a pediatric GI doctor or your pediatrician. Here is a study about constipation and its impact on sleep. Find tips on how to help alleviate constipation here.
Cerebral Folate Deficiency
Cerebral Folate Deficiency (CFD) is a relatively newly identified disorder in which there is low 5-MTHF (5-methyltetrahydrofolate) in the cerebrospinal fluid but normal or even elevated 5-MTHF in the blood. Symptoms of CFD may begin as early as four to six months of age with irritability and sleep problems (insomnia). Treatment options for CFD include folinic acid and a dairy-free diet as mammal’s milk blocks folate receptors. More about CFD can be found here.
Food Sensitivities
An elimination diet can help pinpoint the foods that are causing a problem. Unlike food allergies, food sensitivities cause a delayed reaction. The biggest offenders tend to be dairy, gluten, soy, egg and corn. Here is a chart that shows signs of food sensitivity.
Allergies (Histamine)
Over 90% of food allergies in kids are caused by these eight foods: dairy, egg, soy, wheat, tree nuts, peanuts, shellfish, and fish. Environmental allergies are important as well. Have you ever noticed your child cannot sleep during pollen season? Look into mold, pet dander, pollen, dust, and other environmental triggers. Histamine levels rise at night, which can cause sleep problems. Click here to read a study about sleep and allergies. This article on our blog has some great strategies on how to treat allergies.
Phenols and Salicylates
These properties of food can affect children in many different ways. Some phenols are beneficial from natural foods, but others may be a problem. It is very child specific, and children on the autism spectrum seem to be more susceptible to them. Learn more about phenols, salicylates, and additives here.
Magnesium Deficiency
Doctors rarely test for this but it is critical. A trial of supplementation maybe helpful. Talk to your functional medicine doctor. Read more information about the relationship between low magnesium and sleep issues here and here.
Vitamin D Deficiency
A blood test can determine whether or not your child has low levels of Vitamin D. Here is a study that demonstrates the link between vitamin D and sleep.
Enlarged Adenoids and Tonsils
Enlarged adenoids and tonsils can interfere with both feeding and sleeping. Therefore, consider seeing a pediatric ENT if your child has any of the symptoms listed in this link (snoring, bad breath, cracked lips, episodes of not breathing during sleep, etc.) to determine if they need a sleep study. To read additional studies about the impact enlarged adenoids and tonsils have on sleep, click here and here.
Methyl Donors
The body needs methyl donors to make serotonin. Melatonin is a sleep hormone that depends on serotonin for proper function. Serotonin converts into melatonin in the pineal gland of the brain. Vitamins needed for melatonin production are: 5MTHF (methylfolate), methyl B12, betaine, and other methyl donors. Find more information about methyl donors and their relationship to sleep here.
Cortisol
The adrenal hormone that affects melatonin is cortisol. If cortisol gets too high, melatonin levels drop. In a healthy person, cortisol is highest in the morning so you feel awake. Throughout the day, the levels should slowly drop. However, that pattern is compromised in some people due to adrenal fatigue. During the night, cortisol should raise slowly again. One of cortisol’s functions is to break down glycogen in the liver and turn it to glucose for energy for the morning. If your liver is taxed, you have a hard time doing this conversion. For this reason, liver support may help with sleep, especially if the child cannot stay asleep (supplements that help support the liver include milk thistle, inositol, molybdenum, artichoke, and more). For additional information about the relationship between cortisol and sleep issues, click here and here.
Low Blood Sugar
Many kids that struggle with low blood sugar wake up screaming in the morning or after a nap. They only seem to settle once they have eaten. This also ties into the above comments about cortisol because the liver doesn’t have enough glycogen for energy and the child can wake in the middle of the night as well. Trying a high-protein, high-fat snack before bed like a roll of turkey or a slice of avocado may be helpful. Also, this can be a sign that your child may have mitochondrial dysfunction.
In addition, many parents use an organic “cornstarch slurry” before bed. Cornstarch is a resistant starch and it takes a long time to break down, thus keeping the child fuller longer. 1-2 tablespoons of raw cornstarch mixed into water or juice is typically sufficient. Make sure to use organic!
Parasites
Parasites tend to be active at night. Pinworms, in particular, come out while sleeping. You can shine a flash light on the anus to check for pinworms after the child has fallen asleep.
Candida (Fungal) Overgrowth in the GI Tract
Candida albicans is a fungus (yeast) that can get overgrown and out of balance in the GI tract. While it’s true that everyone has fungus in their GI tract, an overgrowth can disrupt sleep. Besides sleep issues, other symptoms of an overgrowth include: inappropriate laughter, rash or cracking between the toes, white patches in the mouth (thrush), high-pitched squealing, episodes of unexplained/intermittent crying, sugar cravings, etc. Read more about yeast overgrowth here.
GABA – Glutamate Imbalance
GABA is the anti-anxiety neurotransmitter in the brain. Glutamate converts into GABA, as needed, for calming. The GABA shunt can go two ways. It can convert Glutamate into GABA or it can continue to make glutamate which is excitatory. For these reasons, sometimes a diet completely free of glutamate may help improve sleep. To learn more about sleep issues associated with a GABA-Glutamate imbalance, click here and here.
Seizures
Seizures are relatively common in individuals with ASD. Some develop seizures in childhood, some at puberty, and some at adulthood. Although the prevalence of seizures by age is not well studied, recent studies suggest the risk of seizure remains high into adulthood. Many seizures occur at night when we cannot see them, which is why a 24-48 hour EEG is important. You can find more information about seizures here.
GERD/Reflux
GERD (acid reflux) occurs when stomach acid backs up into the esophagus. GERD is painful and can cause your child to wake up in the middle of the night.
Side Effects from Medication
Prescribed medications commonly given to people with autism can significantly impact sleep. Medications such as Risperidone, Abilify, and some prescriptions used to treat ADD/ADHD have side effects that include problems with falling asleep and staying asleep.
Additional Resources
- Introduction to Medical Interventions for Autism
- Underlying Medical Issues in Autism
- Finding a Doctor