Immune Dysfunction in Autism
All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
The body’s immune system defends against infection and protects its own cells. However, research has shown that the immune system is not working properly in many autism cases. Therefore, immune dysfunction is a new area of study in autism.
In fact, this 2022 study showed that people with autism could be dealing with upregulated immune genes leading to brain inflammation. Of the 1275 genes studied, autistic brains had 275 genes that expressed differently than controls. Interestingly, the autism-related expression pattern most closely resembled Alzheimer’s and Parkinson’s immune gene expression pattern.
In addition, this 2023 study showed an altered cytokine profile in adult patients with autism compared to the control group which may indicate immune dysregulation in a subgroup of adult ASD patients.
Lastly, there is new research showing maternal immune dysregulation is a prenatal risk factor for autism spectrum disorder (ASD). In other words, inflammation and metabolic stress on the pregnant mother can result in abnormal cytokine (immune system) signaling and autoimmunity.
But there is good news. There are treatments and lifestyle changes that can help immune dysfunction.
This article will cover:
- Signs of immune dysfunction
- Medical issues in autism caused by immune dysfunction
- Testing for immune dysfunction
- Treatment for immune dysfunction
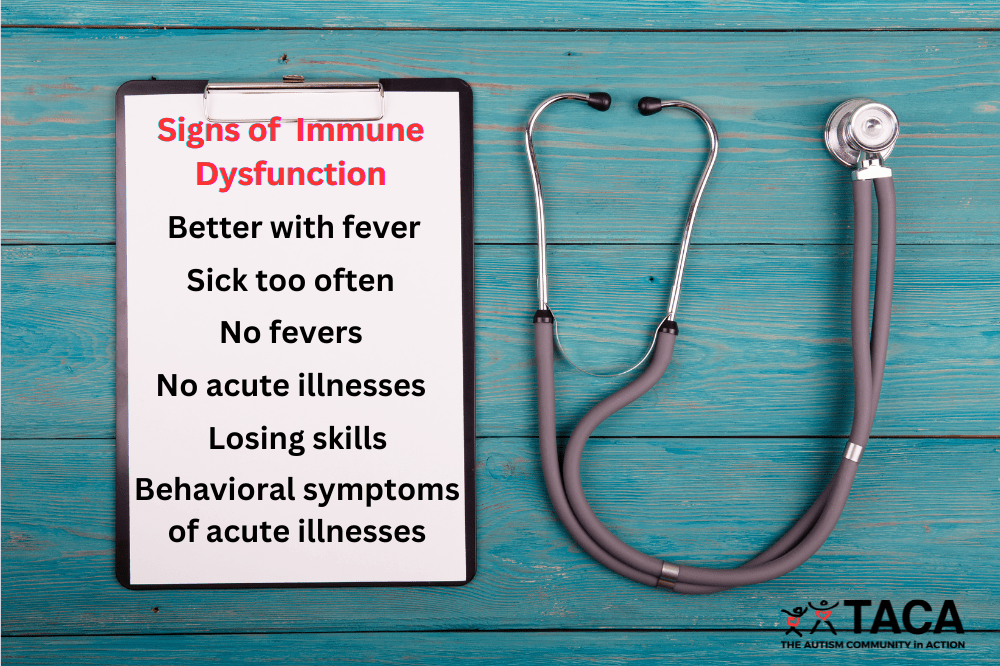
Signs of Immune Dysfunction
There are hints that may point to immune dysfunction in your child. Being observant by journaling can help detect patterns.
Suspect immune dysfunction when your child:
- Has more illnesses than a typical child.
- Does not mount a fever to fight illnesses.
- Does not have typical illness symptoms, but has behavioral issues instead.
- Has skill regression.
- Has improvement of autism symptoms while fevering (often called the “fever effect”).
- Rarely gets sick, even when other household members are sick.
- Has signs of the medical issues listed below.
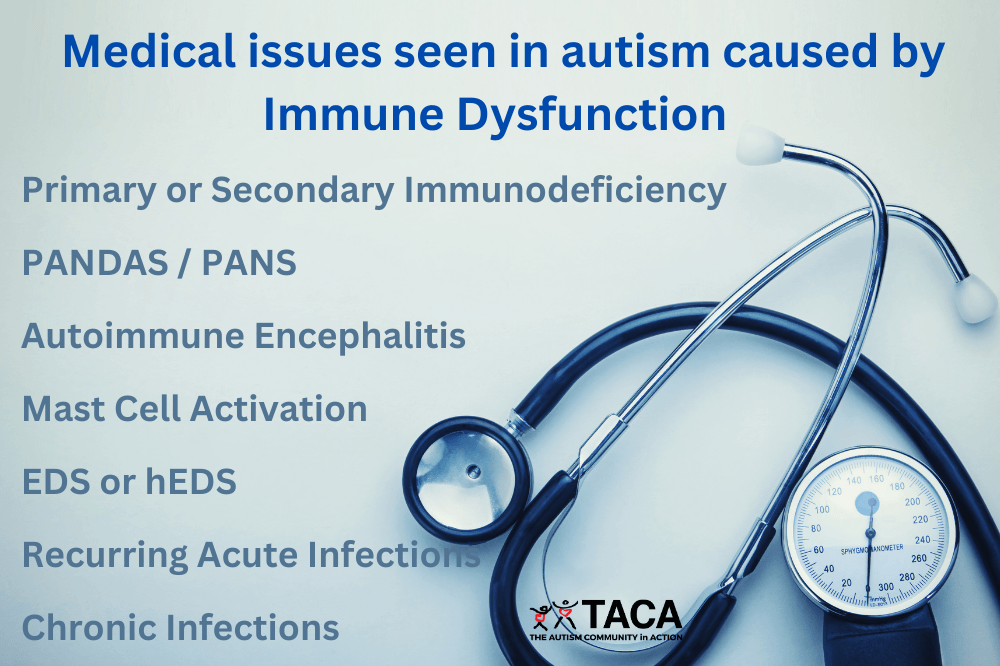
Medical Issues in Autism Caused by Immune Dysfunction
Immune dysfunction seen in autism will manifest as medical issues. Furthermore, these medical issues often have behavioral effects alongside other symtpoms. Examples of some of the common medical issues in autism are listed below.
Primary or secondary immunodeficiency
Primary immunodeficiency happens when the immune system doesn’t work as it should.
Examples of primary immunodeficiency disorders include:
- Common variable immunodeficiency (CVID)
- Severe combined immunodeficiency (SCID)
- Chronic granulomatous disease (CGD)
Secondary immunodeficiency disorders happen when an outside source weakens the body, such as a chemical or infection.
Symptoms of primary or secondary immunodeficiency include:
- Autoimmune disorders
- Anemia
- Delayed growth and development
- Digestive problems
- Frequent illness or infections. For example:
- Pneumonia
- Sinus infections
- Ear infections
- Strep
- Skin infections
Pediatric Autoimmune Neuropsychiatric Disorders associated with Streptococcal Infections (PANDAS)
Pediatric Acute-onset Neuropsychiatric Syndrome (PANS)
PANS / PANDAS is largely an autoimmune disorder, resulting from infections or environmental triggers that cause abnormal activation of the immune system. These infections cause the child to create antibodies which attack the basal ganglia region of the brain causing a whole host of behaviors. However, there are other known causes of PANS as well such as concussions and metabolic issues.
Symptoms include:
- Onset or recurrence of OCD and/or Restrictive eating disorder
- Also, at least one of the following neuropsychiatric symptoms:
- Behavioral/developmental regression
- Deterioration of school performance
- Extreme emotions
- Separation anxiety
- Sensory/motor abnormalities such as handwriting deterioration
- Sleep disturbance (difficulty falling asleep, restless sleep)
- Urinary symptoms (urgency, frequency, bedwetting)
Autoimmune Encephalitis (AE)
Autoimmune encephalitis (AE) occurs when the body’s immune system attacks the brain, causing inflammation. As a result, the immune system produces substances called antibodies that mistakenly attack brain cells. While there is still some debate in the medical community, the current criteria needed for an AE diagnosis is published in this research paper and is also listed below.
Symptoms include:
- Subacute onset (rapid progression of less than 3 months) of:
- Working memory deficits
- Altered mental status
- Psychiatric symptoms
- At least 1 of the following criteria:
- New focal CNS findings
- Seizures or EEG abnormalities not explained by a preexisting disorder
- CSF pleocytosis (white blood cell count of more than 5 cells per mm)
- MRI suggesting brain swelling (encephalitis)
- Other reasons for these symptoms are ruled out.
- Unlike PANS that causes “flares”, these symptoms continue to get worse rapidly.
- Please note that AE can present differently in children.
Mast cell activation
When a resting mast cell is stimulated by an allergic reaction, the mast cell releases its contents of histamine, interleukins, platelet activating factor prostaglandins, proteoglycans, and enzymes. However, over the next 6-24 hours, other inflammatory molecules are released. Mast cell activation disorders range from mildly problematic to severe.
Symptoms include:
- Brain fog
- Diarrhea
- Flushing
- Headaches
- Heart palpitations
- Hives
- Itching
- Low blood pressure
- Muscle pain
- Peripheral neuropathy (numbness, tingling)
- Shortness of breath
- Skin sensitivity to hygiene products or topicals
Ehlers-Danlos syndrome (EDS) or Hypermobile Ehlers-Danlos syndrome (hEDS)
Ehlers-Danlos syndrome (EDS) affects your connective tissues — primarily your skin, joints and blood vessel walls.
Hypermobile Ehlers-Danlos syndrome (hEDS) is a less severe form of EDS causing joint hypermobility. This is a result of defects in the collagen protein.
Symptoms include:
- Easy bruising
- Flat feet
- Inflammatory bowel disease
- Joint hyper mobility
- Muscle or bone pain
- Muscle weakness
- Stretchy skin
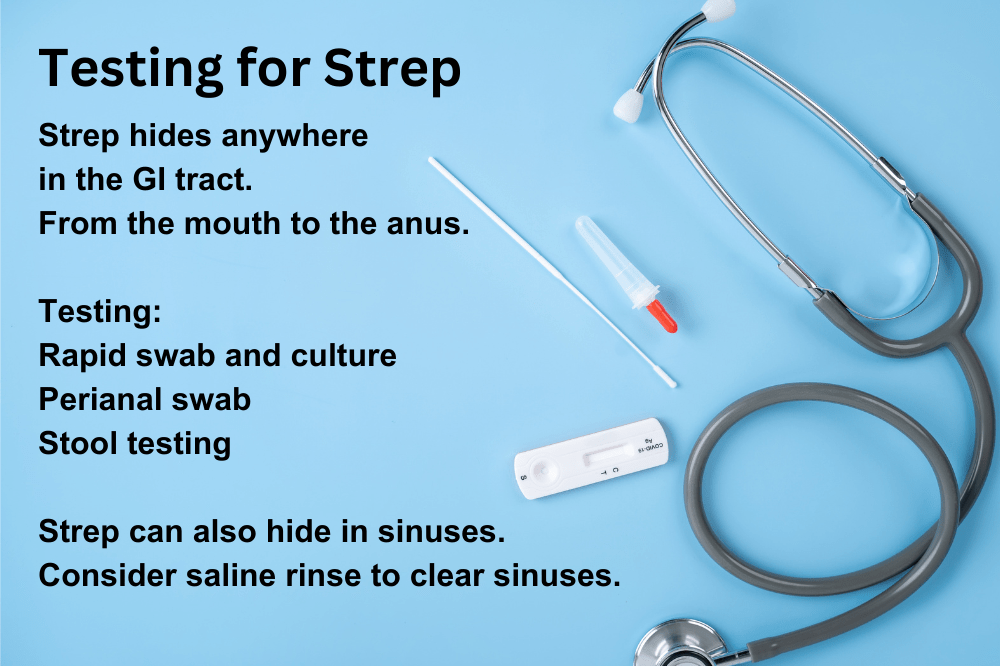
Recurring Acute Infections
Infections can cause inflammation in the body. In addition, when we treat with antibiotics, the bacteria or virus may hide under biofilms only to resurface often.
Examples of recurring acute infections are:
- Strep
- Look for strawberry tongue, red anal ring, peeling fingers/feet, enlarged tonsils/adenoids.
- Mycoplasma
- Look for fatigue
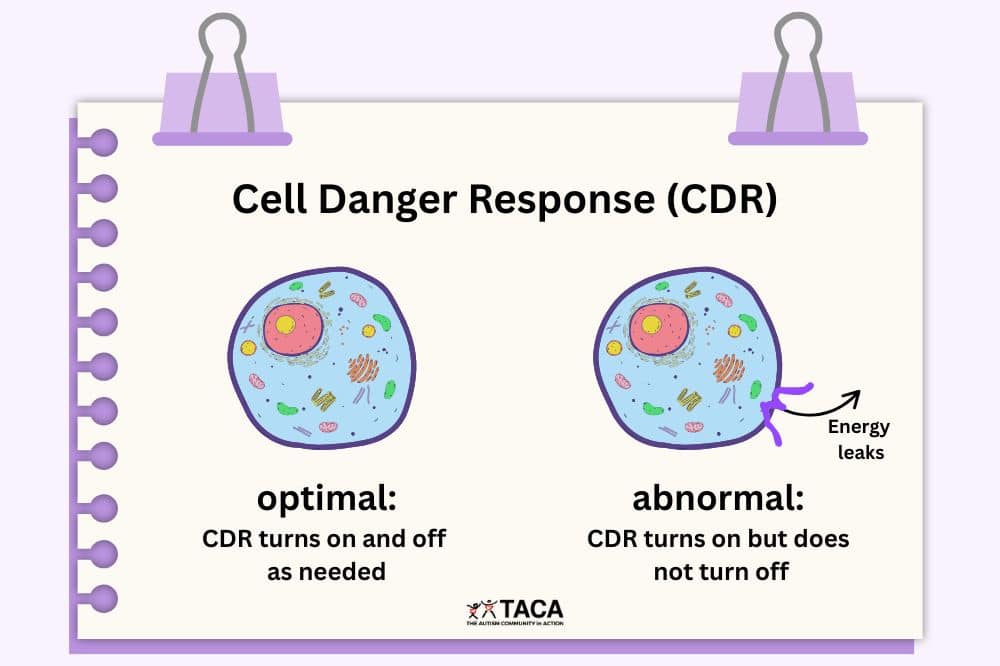
Persistent chronic infections
When the body does not mount a proper response to an infection or virus, it does not fight off the acute illness as it should. Consequently, the infection or bacteria is left festering in the body wreaking havoc on the immune system.
Examples of such chronic infections are:
- Lyme and/or Lyme co-infections
- Symptoms listed in this TACA article titled “Lyme and Autism“.
- Bartonella
- Look for swollen glands around the head.
- Additionally, look for unusual streak rash that looks like stretch mark.
- Finally, rage is a known symptom of Bartonella.
- Babesia
- Look for unusual sweating at night, fatigue, and nausea.
- COVID
- Look for brain fog, dizziness upon standing, and/or extreme fatigue.
- Herpes family infections
- Epstein–Barr virus (EBV)
- Look for swollen lymph nodes, extreme fatigue.
- Cytomegalovirus (CMV)
- Look for swollen lymph nodes, fatigue, and nausea.
- HHV6 (most common symptom is Roseola)
- Look for fatigue, abdominal pain, sore throat that comes and goes.
- Herpes Simplex Virus 1 & 2
- Look for mouth sores/ulcers.
- Varicella (Chickenpox)
- Look for numbness in hands or feet, fatigue, possible random rashes or spots.
- Epstein–Barr virus (EBV)
- Parasitic infections
- All parasitic infections have different symtpoms.
- Look for low iron and high eosinophils without allergic reactions.
- Candida overgrowth
- Look for Thrush (white tongue)
- Additionally, there are many behavioral signs of yeast. Learn more in the TACA article on “Yeast Overgrowth in Autism“.
Testing for Immune Dysfunction
A full workup of your child is necessary. See the following list of tests that may be run by your immunologist or functional medicine provider to uncover what the body may be dealing with. Specifically, the particular tests run will depend on what symptoms are displayed.
- CBC
- Platelets
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
- Oxidative Stress markers
- 8OH Deoxyguanosine, Lipid peroxides, Malonodialdehyde
- Total immunoglobin profile
- IgG and IgG subclasses, IgE, IgA, and IgM
- White Blood Cell Count (WBC)
- T lymphocyte panel – CD4/CD8
- ANA
- Vit D level
- Zinc level (test alongside copper level)
- Testing for specific infections
- Both IgM (current infection) and IgG (past infection)
- S-100B (serum)
- Tests blood brain barrier permeability
- Cytokine panels
- Quest Diagnostics – Encephalitis antibody evaluation
- Covered by health insurance
- Cunningham Panel
- Not covered by insurance
- Mayo Encephalitis Panel
- Covered by insurance but requires a specific draw method
- Adults: Encephalopathy, Autoimmune/Paraneoplastic Evaluation, Serum
- Children: PCDES / Pediatric Autoimmune Encephalopathy/CNS Disorder Evaluation, Serum
- Quest Diagnostics – Encephalitis antibody evaluation
- Cytokine testing such as:
- IL-1
- Elevated with Candida
- IL-6
- Elevated with PANDAS
- IL-17
- Elevated with PANDAS, Candida
- IL-8
- Elevated with Clostridia
- IL-1
- NLRP
- Elevated with Candida
- LPS
- Elevated with Gram Negative Bacteria
- Detects leaky gut
- D-dimer
- Looks for protein fragments of blood clots
- Nasal swab for MARCoNS
- Celiac panel
- Thyroid Peroxidase antibodies
- NMDA antibodies
- GAD65 antibodies
- If necessary, an autoimmune encephalopathy workup via lumbar puncture
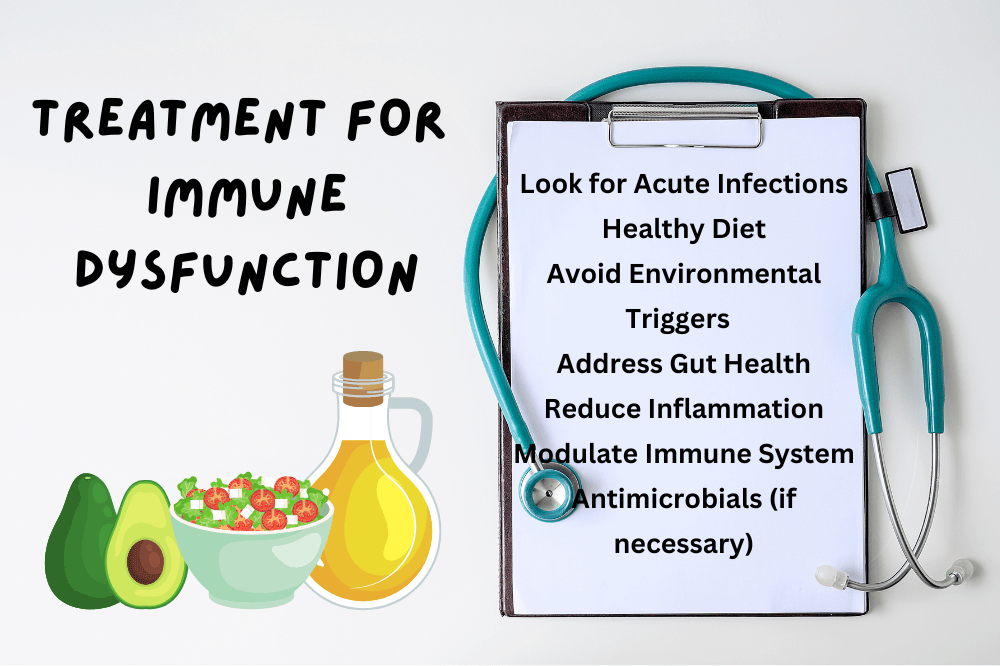
Treatment for Immune Dysfunction
Effective treatment for immune dysfunction requires a multi-pronged approach. Overall, the goal is to figure out your child’s trigger(s), sensitivities, and clean up the environment.
Look for acute infections that we may not be able to see. If found, treat.
- Sinuses, ears, tonsils, adenoids
- Urinary tract, bladder, or kidney infection
- Skin infection
- Gut infection
- Tooth infection
Pay attention to Diet
- Mediterranean Diet
- Anti-inflammatory foods
- Lots of fruits and vegetables
- Low sugar or no sugar
- Maximize antioxidants
- No excitotoxins (MSG, caffeine, food dyes, additives)
- GMO free
- Filtered water
- Foods that are prebiotics
- High fiber diet
- Spices
- Foods that have probiotics (fermented foods)
- Diverse diet in order to diversify the gut flora
Avoid Environmental Triggers
- Fragrances
- Pollution
- Smokers
- Chemicals in the air
- Mold in the house or school
Address Gut Health
- Check for constipation with an x-ray
- Bowel cleanse if needed
- Use enzymes as needed
- Pancreatic, digestive enzymes
- Support the liver for proper bile output
- Address Biofilms
- Use prebiotics or probiotics depending on stool testing results:
- Too much Bacteroides, Allistipes, parabacteroides, Prevotella indicates a need for:
- High fiber diet
- No inulin
- Not enough Bacteroides, Allistipes, parabacteroides, Prevotella indicates a need for:
- Inulin (short-term only)
- Animal based protein
- S. Boulardii
- Too much Bacillus, Clostridium, Enterococcus, Lactobacillus, Ruminoccocus indicates a need for:
- Lactulose
- High Bifido requires berberine
- High Clostridia requires Carnitine, S. Boulardii, High dose probiotics
- Not enough Bacillus, Clostridium, Enterococcus, Lactobacillus, Ruminoccocus indicates a need for:
- Inulin
- Plant based diet
- Resistant starches
- Lactobacillus Rhamnosus (gg)
- Bifido Logum
- Too much Bacteroides, Allistipes, parabacteroides, Prevotella indicates a need for:
Supplements to Reduce Inflammation
- Resveratrol
- Boswellia
- Curcumin
- Fish Oil (Omega 3 fatty acids)
- Aloe (certified)
- Pycnogenol
- Ashwagandha
- Berberine
- PEA
Nutrients used for Immunoregulation
- Zinc (very important)
- Vitamin A (very important)
- Vitamin D (very important)
- Blood levels should be between 50-80
- Iron
- Selenium
- Molybdenum
- Vitamin B1
- Needed to get sugar into the mitochondria for energy
- B2
- Vitamin B6
- Folinic acid or 5MTHF
- Never folic acid
- Vitamin B12
- Vitamin C
- Vitamin E
Other Anti-inflammatory Treatments
- Steroids (short term bursts only)
- IVIG
- Anti-seizure medication such as Lamictal, Depakote, Keppra
- LDI (Low dose Immunotherapy)
- Camel’s milk
Immune Modulators
In autism, the idea is not to boost the immune system, but rather, to modulate it. These products are known to do that.
- Vitamin D
- IVIG
- Helminth Therapy
- Low Dose Naltrexone (LDN)
- Hyperbaric Oxygen treatment
- Lauricidin
- Amantadine
Antimicrobials (depending on trigger)
- Antibiotics
- Antiviral medication (Valtrex)
- Antiparasitic (Alinia)
- Herbals:
- Goldenseal
- Neem
- Berberine
- Olive Leaf Extract
Conclusion
Immune dysfunction is commonly found in autism. Therefore, if you suspect immune system problems in your child, it is important to find an open-minded doctor to work with you and test your child properly. Consequently, the lab results will help guide treatment. Remember that there are often triggers for immune dysfunction. Finding and then treating those triggers is paramount to improved health. Coupling that with a protocol to lower overall inflammation will give optimal outcomes.