Do Parents Need Therapy Too?

All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
As parents, we tend to neglect ourselves when raising our children. Healing ourselves, however, is one of the most important pieces of parenting our kids with autism. Parents must be healthy in order to provide a supportive and hopeful home environment. Additionally, our kids can feel our energy, and that energy should be positive. We hear about helping ourselves frequently with references to the importance of self-care. In spite of this, parents’ mental health gets overlooked due to the day-to-day pressures and sense of overwhelm that often accompany an autism diagnosis. Extensive research has shown parents of children with autism have more mental health difficulties compared to other parents. It is key to recognize signs of depression and anxiety in yourself. Prioritizing your own mental health and seeking professional therapy to manage chronic stress is a critical investment in the effectiveness of intervention and child outcomes.
This article will cover:
- What depression looks like in parents
- What anxiety looks like in parents
- Different types of trauma
- How to locate a therapist for yourself, as the parent
Depression
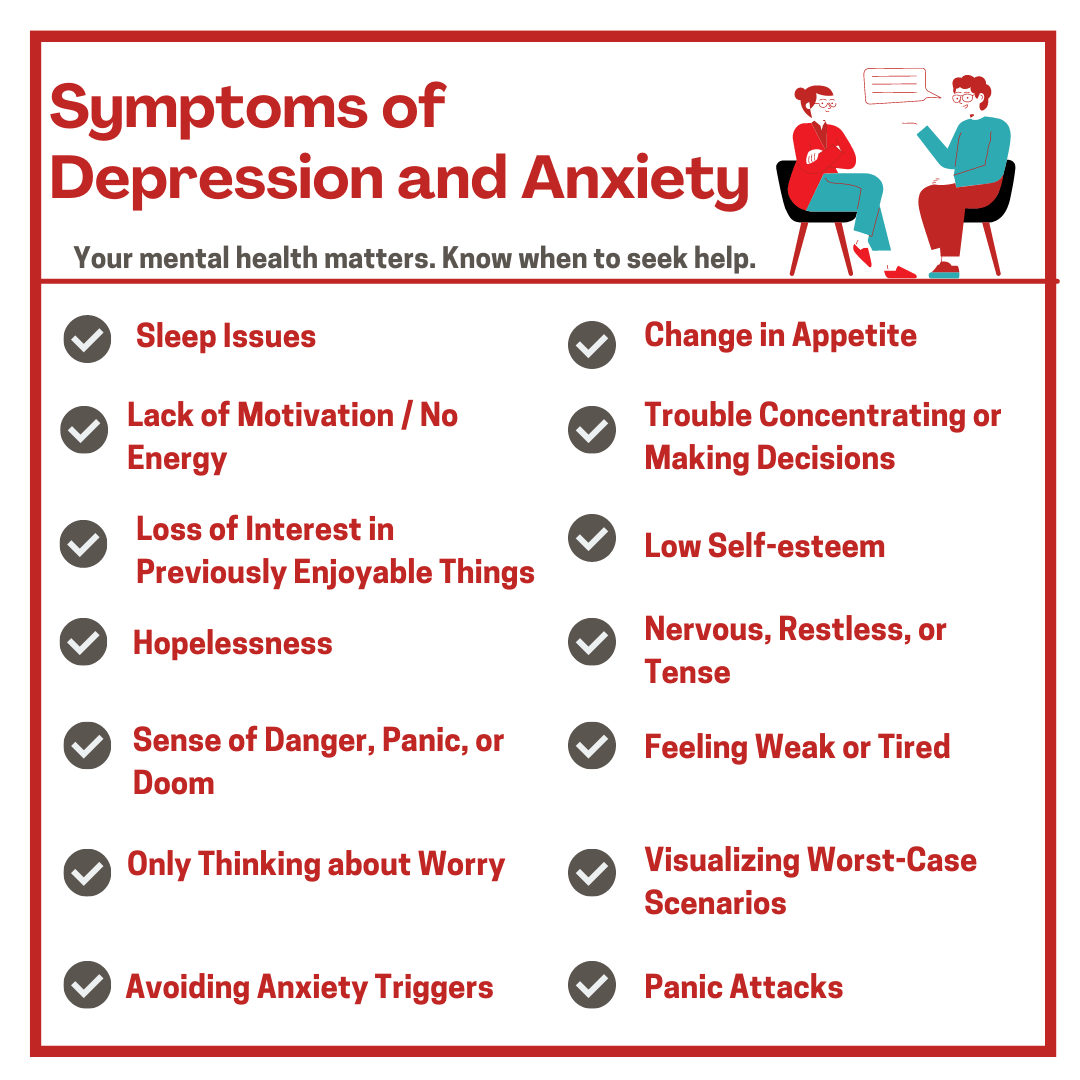
Do these symptoms sound familiar?
- Sleeping too much (hypersomnia) or sleeping too little (insomnia)
- Parents of children with Autism often experience disruptions in their own sleep due to the sleep issues of their children.
- Parents may find themselves sleeping excessively when not caregiving due to exhaustion. Also, they may sleep to escape stress and overwhelming emotions.
- Eating too much or eating too little
- Chronic stress can cause loss of appetite or can cause us to adopt overeating as a coping mechanism.
- Low energy (fatigue) or lack of motivation
- Maintaining day-to-day routines and navigating obstacles can be exhausting. As a result, this depletes mental and physical reserves.
- Trouble concentrating or struggling to make decisions
- Overwhelm, chronic stress and undiagnosed medical conditions contribute to poor focus, memory, and ability to multi-task.
- Steep learning curves, information overload, or conversely, a lack of clear answers can lead to uncertainty about the best course of action for your child.
- Loss of interest in previously enjoyed motivators and hobbies
- Parents may become consumed in helping their children and find themselves without time or energy to nurture their own identities and happiness.
- There may be a degree of guilt that accompanies taking time for self.
- Low self-esteem
- Feeling a sense of inadequacy or despair at being unable to meet their child’s needs, address medical problems, and handle difficult behaviors can feel defeating.
- Hopelessness
The above symptoms are all characteristic of Depression, which can be helped tremendously by professional counseling. Several meta-analyses have shown the effectiveness of different psychotherapies in reducing symptoms of depression compared with control conditions. In fact, a meta-analysis of 331 randomized trials showed that all therapies were universally more effective than care-as-usual.
Still not sure if Depression might be a concern for you? Try taking the Beck Depression Inventory or the Zung Self-Rating Depression Scale.
Anxiety

Do these symptoms sound familiar?
- Feeling nervous, restless, or tense
- Parents of children with autism and complex medical needs are frequently required to adapt to unpredictable circumstances. When we do not feel in control or prepared, we often become overwhelmed by a sense of worry.
- Having a sense of impending danger, panic, or doom
- Hypervigilance is common for most parents in the early years of raising children. In typical circumstances, this fades as experience and observation teach us that we can trust our children to make safe choices and trust our abilities to protect them. For autism parents, life experience may not follow this path. Instead, we learn that we must be constantly watching and ready.
- Feeling weak or tired
- Exhaustion from the combined pressure of parenting and carrying the weight of worry leaves parents with little physical and emotional energy.
- Trouble concentrating or thinking about anything other than the current worry
- The mind is wired to solve problems to reach a peaceful state. Sometimes we get stuck in a problem-solving mode when we are constantly exposed to complex scenarios without easy or concrete answers.
- Nightmares or trouble sleeping
- The problem-solving and answer-seeking of the day often follow us into the night. When we can’t find a solution to a problem, we start writing stories with our imaginations to prepare ourselves for the potentially negative outcome.
- Catastrophizing, or visualizing worst-case scenarios
- Parents that are stuck in problem-solving mode for long periods of time may begin to achieve a sense of preparedness by mentally preparing for the worst-case scenario. No one wants to be blindsided, and this is the minds way of avoiding that.
- Having the urge to avoid things that trigger anxiety
- Understandably, when parents become overwhelmed with anxiety, they seek to avoid it.
- Symptoms of a “panic attack”
- Rapid heart rate
- Flushing or feeling hot
- Sweating or chills
- Trembling
- Trouble breathing
- Chest pain
- Weakness
- Tingly or numb hands
Anxiety and chronic stress go hand-in-hand. Certainly, they have long-term effects on physical health. External triggers typically cause stress. Conversely, internal triggers typically cause anxiety. During these moments, your body kicks its sympathetic nervous system into gear to prepare you to manage the trigger. When this happens, we refer to it as “Fight or Flight”. When the body’s response to stress doesn’t go away after a situation has passed, or if it appears without a stressful event occurring, then you may be experiencing anxiety. For people with anxiety, the body reacts to internal triggers (like various worries or unsolved problems) as if a stressful or dangerous event is taking place which can lead to ongoing physical symptoms.
Anxiety is the most common mental health disorder as approximately one-third of the population will be affected by an anxiety disorder during their lifetime. Many of our children also suffer from anxiety. Addressing it medically and therapeutically is a family investment in long term physical health. Many of the same things that help our children with anxiety are also supportive for us.
Still not sure if Anxiety might be a concern for you? Try taking the Zung Self-Rating Anxiety Scale, or the GAD-7.
What is Trauma, Really?

Somewhere in the middle of anxiety and depression, and weaving in and out of both is trauma. Trauma is often a misunderstood concept that makes people think of war, natural disasters, violent crime, and abuse. While these are all traumas, the true definition involves far more than we often allow ourselves to acknowledge. In psychological terms, trauma is a response to an event that is out of our mental capacity to cope and process. This includes grief over the dreamed future that did not come true. This also includes the loss associated with regression – either initial or incrementally ongoing. In addition, it includes the deep desire to feel the emotional and physical bond with your child reciprocated. Lastly, this includes coping with the ongoing and sometimes constant situations associated with the behavioral symptoms of autism, including aggression.
- Big T Trauma vs. little t trauma
- Big T traumatic events are generally life-threatening and highly disturbing.
- Little t trauma consists of events, situations, or ongoing circumstances that cause distress, fear, hopelessness, or helplessness. Little t trauma is cumulative. It often goes unrecognized and therefore untreated. The collective impact of these traumas can cause significant psychological distress and harm.
- Complex Trauma
- As mentioned above, trauma is cumulative. Our past experiences influence how we perceive and interact with the world as adults and as parents. If our life experience from childhood is troubling and traumatic, we have less room to emotionally tolerate further trauma in adulthood. Particularly if the trauma has similar themes like hopelessness, lack of control, rejection and isolation, shame, or guilt.
- Complex trauma can also develop from repeated exposure to initial traumas as an adult, through persistent re-exposure. This can happen when children regress and recover in an ongoing pattern (PANS/PANDAS for example), or where aggression is involved.
- Attachment Trauma
- Defined as a consistent disruption of physical and emotional safety inside the family system. Our nervous systems are constantly adapting and learning how to maintain a safe connection with others. When that connection is unsafe or unavailable – it can cause problematic relationships.
- Moreover, attachment trauma is linked to our overall mental health and is closely related to Complex Trauma. Complications include being hyperreactive to stress and becoming engrossed in our relationships to the point of losing our sense of self.
- Medical Trauma
- Results from a set of physical and mental responses to treatment experiences both for ourselves and our children. It includes the emotional response that comes from seeing our children experiencing pain or discomfort due to medical conditions either at home or in a medical setting.
- Medical trauma may also present in scenarios where a lack of provider knowledge of up-to-date research causes professionals to minimize or disregard symptoms. This may include refusing to run lab or diagnostic testing and dismissing legitimate clinical concerns as being related to a mental health diagnosis. “It’s just Autism.”
Still not sure if trauma might be a concern for you? Try taking the PCL-5 or the ACE.
How to Find Therapy
It is a big step to acknowledge that you, as the parent, would benefit from therapy. However, it has the potential to make you a much better parent. And that, in turn, will help your child immensely. If you are experiencing depression, anxiety, and/or trauma, here are some ways to find a therapist:
- Reach out to local Autism support groups for recommendations on Licensed Counselors or Counseling Psychologists in your area.
- Visit Psychology Today for a comprehensive listing of mental health providers in your area.
- Explore employer benefits to see if therapy is an option (EAP).
- If you are a student, your school may provide access to a counseling center.
- Watch this clip on signs you are struggling and different types of therapy from TACA’s 2021 National Conference on “Brain-Based Strategies for Parenting” with Nicole Saylor Ph.D.